Session Information
Date: Sunday, November 7, 2021
Title: Epidemiology & Public Health Poster II: Inflammatory Arthritis – RA, SpA, & Gout (0560–0593)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Increasing evidence implicates respiratory mucosa in the pathogenesis of rheumatoid arthritis (RA). However, individual respiratory tract diseases, especially of the upper airways, sinuses, and pharynx, have remained relatively understudied for RA risk. We aimed to determine whether specific respiratory tract diseases are associated with rheumatoid arthritis RA development.
Methods: This case-control study was performed within a large, single center biobank. We matched newly diagnosed RA cases to three controls on age, sex, and electronic health record (EHR) history. We identified RA using a validated algorithm incorporating diagnosis codes, medications, and natural language processing, and then confirmed cases by medical record review. We confirmed date of RA diagnosis by medical record review and obtained RA serostatus from clinical laboratory results. “Seropositive” RA included positivity for rheumatoid factor and/or anti-citrullinated protein antibodies. Respiratory tract disease exposure required one inpatient or two outpatient codes two years before index date of RA or matched date (mean positive predictive value 86%). We obtained covariates including smoking status and pack-years from the biobank survey, supplemented by electronic health record data. Conditional logistic regression models calculated odds ratios (OR) for RA with 95% confidence intervals (CI), adjusting for potential confounders including age, sex, length of EHR history, biobank enrollment year, race/ethnicity, education, body mass index, smoking status, and smoking pack-years. We then stratified by serostatus and smoking.
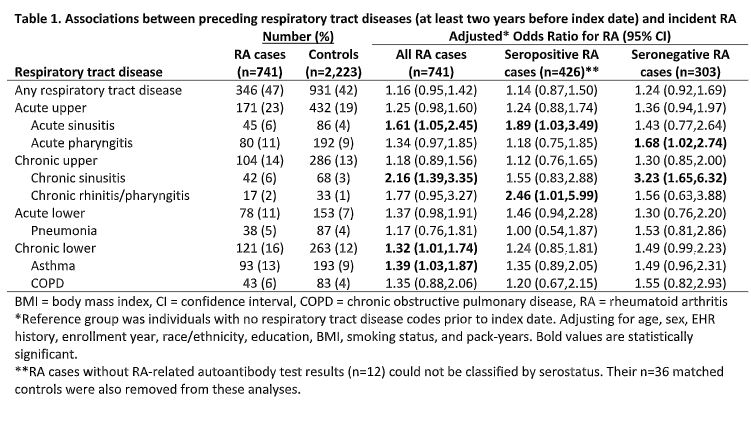
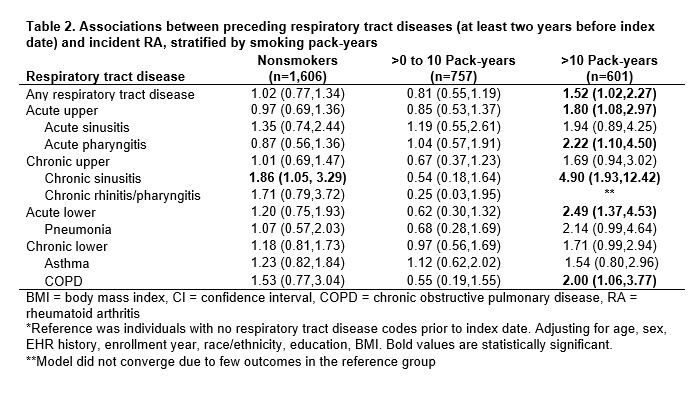
Results: We identified 741 newly diagnosed RA cases and 2,223 controls (both median age 55, 76% female). In the pre-index exposure period, any respiratory tract disease was present in 47% of cases and 42% of controls. Acute sinusitis (OR 1.61, 95% CI:1.05,2.45), chronic sinusitis (OR 2.16, 95% CI:1.39,3.35), and asthma (OR 1.39, 95% CI:1.03,1.87) were associated with increased risk of RA diagnosis (Table 1). Acute respiratory tract disease burden during the pre-index exposure period was also associated with increased RA risk (OR 1.30 per 10 diagnosis codes, 95% CI:1.08,1.55). Acute pharyngitis was associated with seronegative RA (OR 1.68, 95% CI:1.02,2.74) but not seropositive RA; chronic rhinitis/pharyngitis was associated with seropositive RA (OR 2.46, 95% CI:1.01,5.99) but not seronegative RA. Respiratory tract diseases tended towards higher associations with RA in smokers, especially >10 pack-years (OR 1.52, 95% CI:1.02,2.27; p 0.10 for interaction; Table 2).
Conclusion: We identified novel associations of acute/chronic sinusitis, pharyngitis, and acute respiratory tract disease burden with RA risk. These results suggest that the mucosal paradigm of RA pathogenesis may not only involve the lower respiratory tract, but also the upper respiratory tract.
To cite this abstract in AMA style:
Kronzer V, Huang W, Zaccardelli A, Crowson C, Davis J, Vassallo R, Doyle T, Losina E, Sparks J. Associations of Sinusitis, Pharyngitis, and Respiratory Tract Disease Burden with Incident Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/associations-of-sinusitis-pharyngitis-and-respiratory-tract-disease-burden-with-incident-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-sinusitis-pharyngitis-and-respiratory-tract-disease-burden-with-incident-rheumatoid-arthritis/