Session Information
Date: Monday, November 8, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster II (1364–1390)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: The gastrointestinal (GI) tract is the most commonly affected internal organ in systemic sclerosis (SSc). SSc GI disease is heterogeneous, with some patients experiencing only mild acid reflux, while others progress to severe GI disease requiring total parenteral nutrition to sustain life.1–3 As our understanding of disease pathogenesis is poor and risk stratification tools in SSc GI disease are limited, we sought to determine whether distinct types of esophageal dysfunction associate with specific clinical phenotypes and outcomes in SSc.
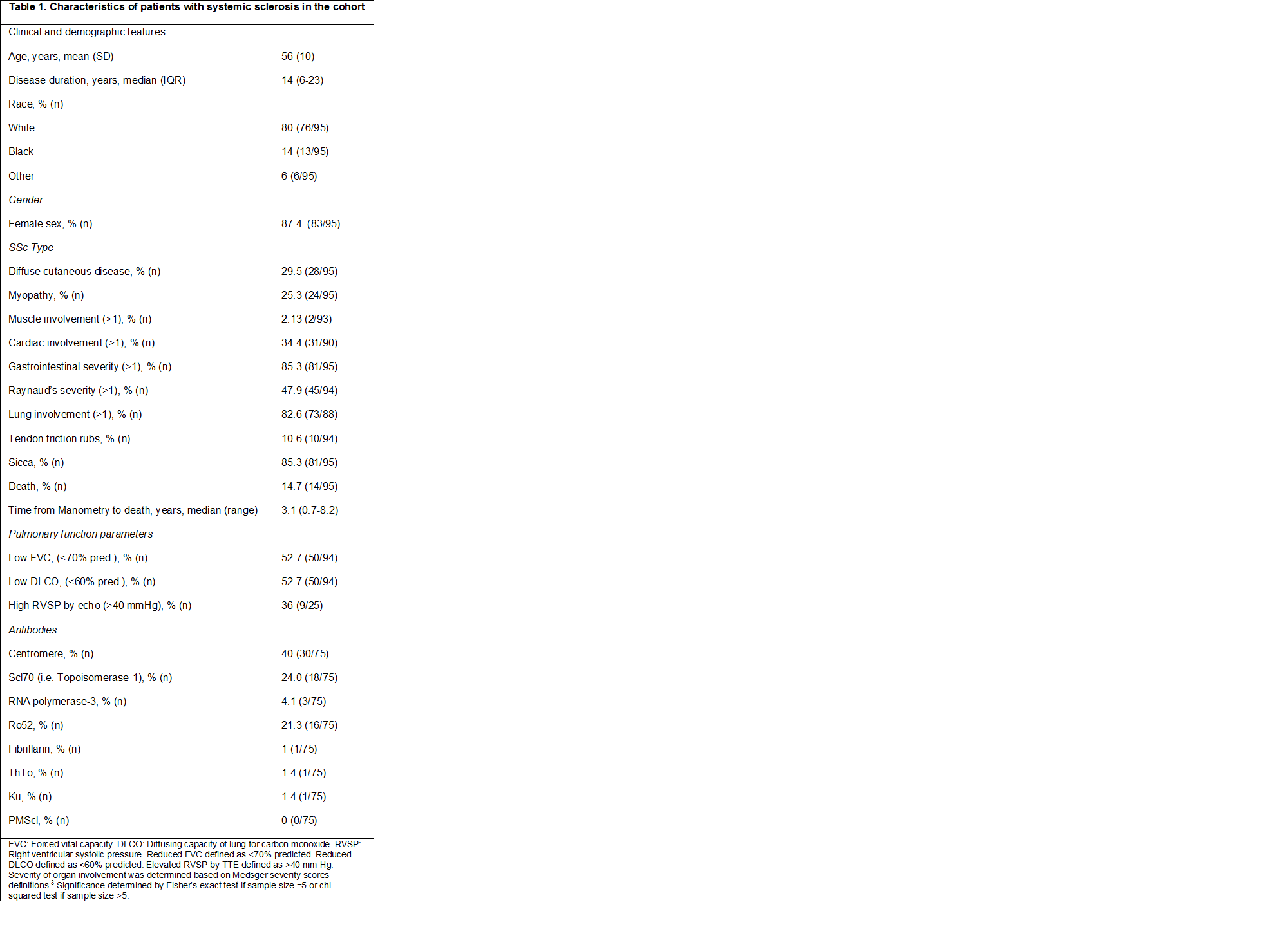
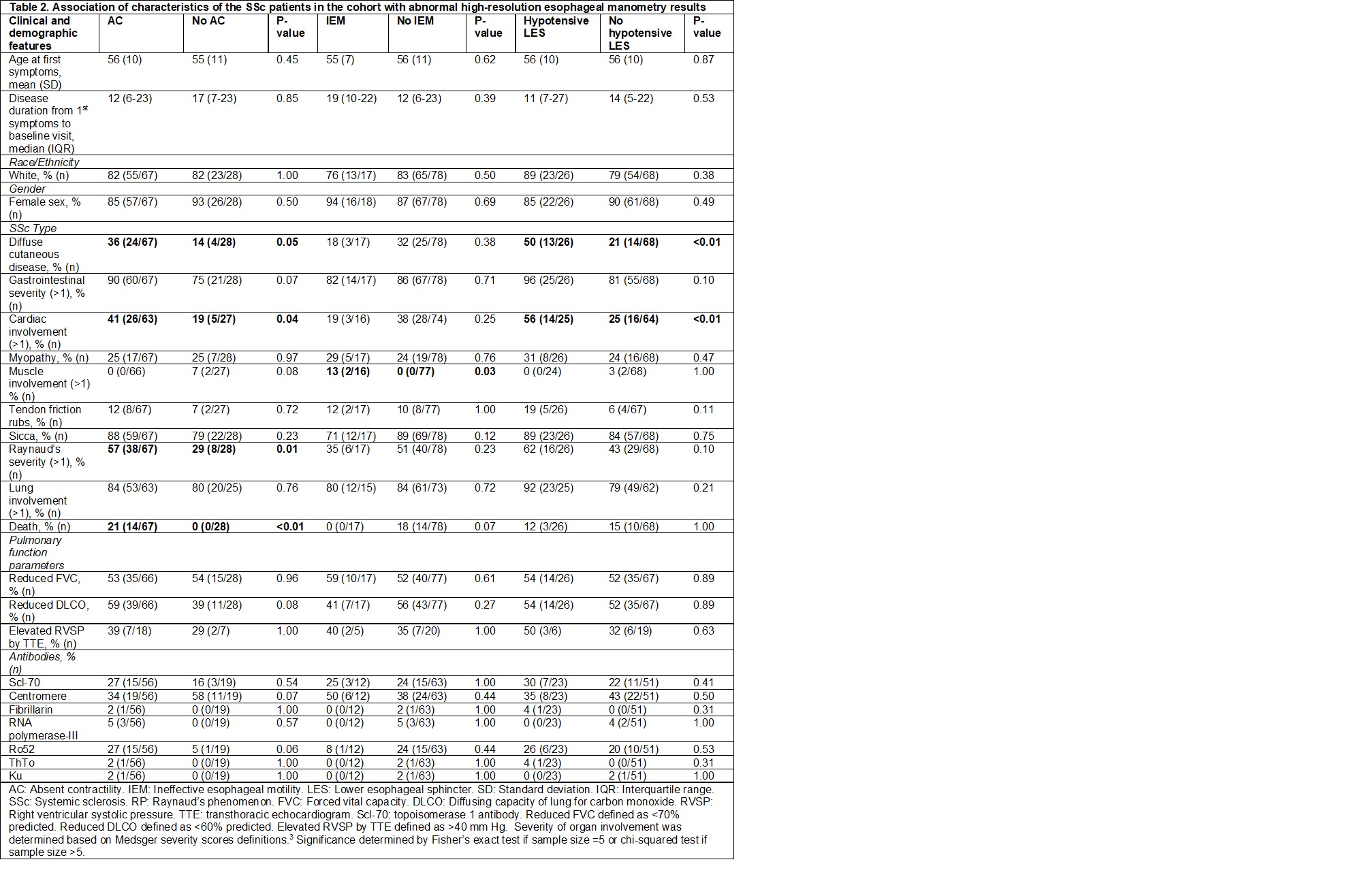
Methods: Patients in the Scleroderma Center Research Registry who had high resolution esophageal manometry (HRM) studies completed in our hospital system as part of their clinical care between 2011 and 2020 were identified through our Precision Medicine Analytics Platform. Data from the manometry reports were downloaded, abstracted, and merged with existing demographic, clinical and serologic data that had been collected longitudinally from 1991-2020 as part of our Center’s Research Registry. Associations between esophageal abnormalities identified on manometry [absent contractility (AC), ineffective esophageal motility (IEM), hypotensive LES (hypoLES)] and patient demographics, clinical characteristics, and autoantibody profiles were examined.
Results: Ninety-five patients with SSc had HRM data. Of these patients, 67 patients (71%) had AC (44 patients with only AC, 23 patients with AC and a hypoLES), 17 patients (18%) had IEM (3 with a hypoLES), and 11 patients (12%) had normal studies. Median disease duration in patients with AC was 12 years (6-23) and in patients with IEM was 19 years (10-22). The presence of AC was significantly associated with diffuse cutaneous disease (36% vs. 14%; p=0.05), more severe cardiac involvement (Medsger score >1; 41% vs. 19%; p=0.04), and more severe Raynaud’s phenomenon (Medsger score >1; 57% vs. 29%, p=0.01). AC was seen in 100% of the patients in the study that died (14/14, p< 0.01). Among patients with AC, 21% died, whereas none of the patients without AC died (p< 0.01). Interestingly, 93% (15/16) of Ro52 positive patients had AC (p=0.06). These findings were not seen in patients with IEM.
Conclusion: In patients with SSc who are referred for manometry, the presence of AC, but not IEM, is strongly associated with a severe clinical phenotype and a high risk of death. Further prospective studies are needed to assess the prevalence of AC in early disease, the timing of its onset relative to other end organ complications, and its rate of progression among patients with SSc.
References:
1. Mayes MD, Lacey J v., Beebe-Dimmer J, et al. Prevalence, incidence, survival, and disease characteristics of systemic sclerosis in a large US population. Arthritis and Rheumatism. 2003;48(8).
2. Al-Dhaher FF, Pope JE, Ouimet JM. Determinants of Morbidity and Mortality of Systemic Sclerosis in Canada. Seminars in Arthritis and Rheumatism. 2010;39(4).
3. Medsger TA, Silman AJ, Steen VD, et al. A disease severity scale for systemic sclerosis: Development and testing. Journal of Rheumatology. 1999;26(10).
To cite this abstract in AMA style:
Tucker A, Perin J, Volkmann E, Shah A, Pandolfino J, McMahan Z. Associations of Esophageal Dysmotility Patterns with Extra-intestinal Features in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/associations-of-esophageal-dysmotility-patterns-with-extra-intestinal-features-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/associations-of-esophageal-dysmotility-patterns-with-extra-intestinal-features-in-patients-with-systemic-sclerosis/