Session Information
Date: Monday, November 9, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Bench to Bedside
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty, an emerging concept in SLE, represents an individual’s ability to respond to physiologic stress. The first lupus-specific frailty index, the SLICC-FI, was recently shown to predict mortality and damage accrual in the SLICC disease inception cohort. Multiple studies confirm that telomere length is significantly shorter in patients with SLE, however there is conflicting evidence regarding the role of telomeres in mediating frailty in the geriatric population. The objectives of this study were 1) to assess if frail patients with SLE have shorter telomere length compared to non-frail patients and 2) to examine the relationship between telomere length and changes in frailty over time.
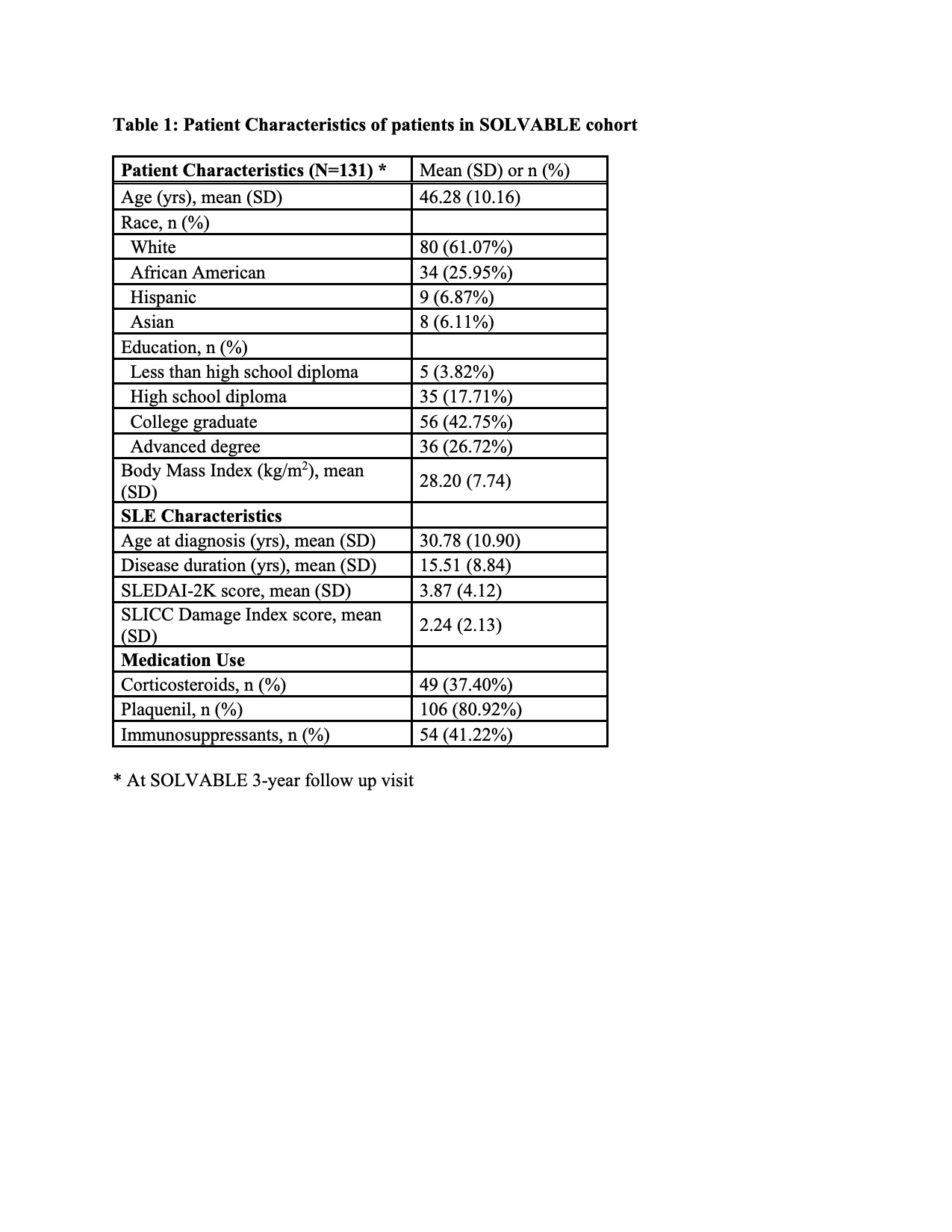
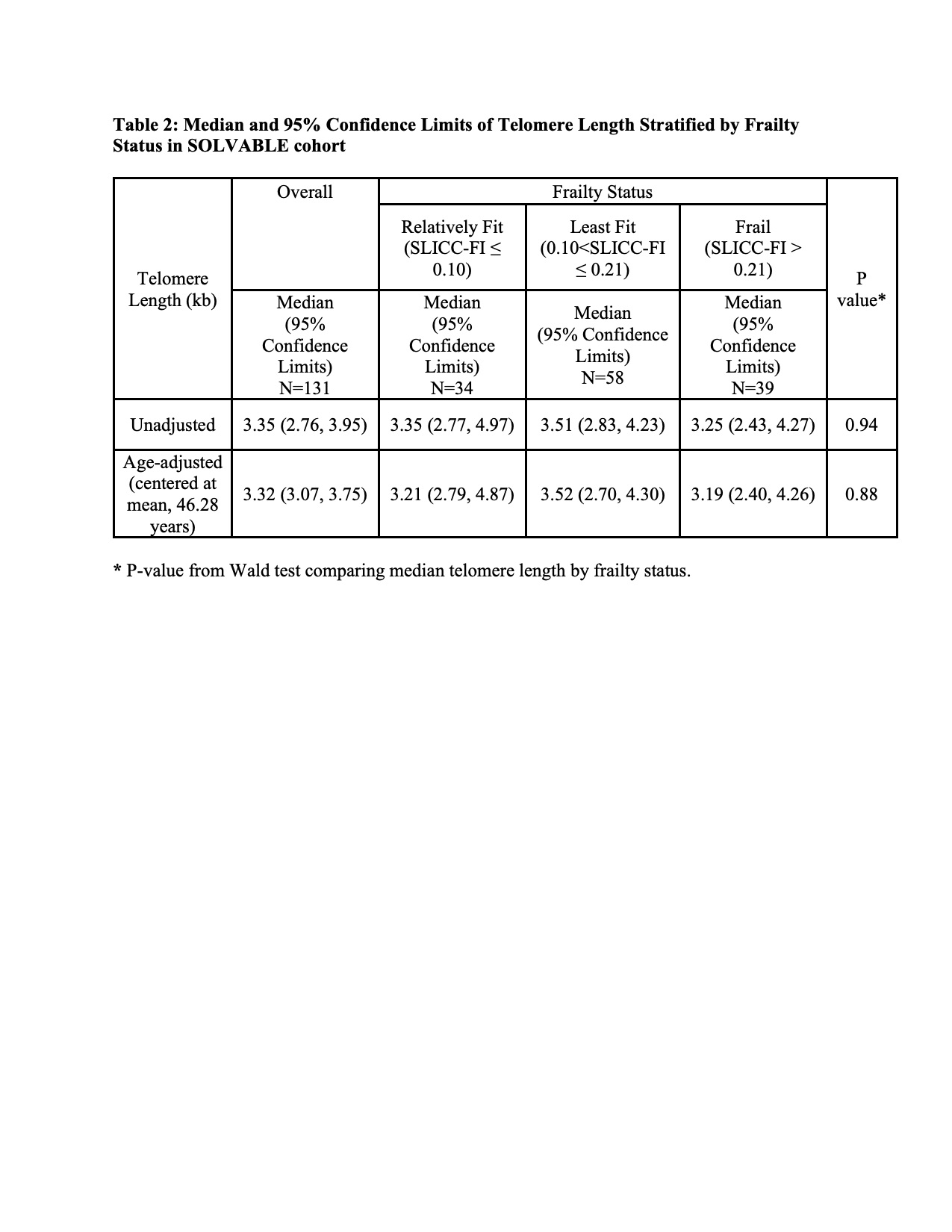
Methods: Data was analyzed from 131 of 185 adult women who met the following criteria: 1) 1997 revised ACR criteria for definite lupus, 2) enrolled in the Study of Lupus Vascular and Bone Long-Term Endpoints (SOLVABLE) cohort consisting of adult women from the Chicago Lupus Database and 3) telomere length measured from whole blood by PCR at 3-year follow up visit, which is the baseline time point for this study. Adapted SLICC-FI scores consisting of 46 health deficits were calculated at baseline (3-year follow-up visit) and 2 years after baseline (5-year follow-up visit). Using baseline SLICC-FI scores, patients were categorized as frail (SLICC-FI >0.21), least fit (0.10< SLICC-FI≤0.21) or relatively fit (SLICC-FI ≤0.10). We used median quantile regression models to calculate unadjusted and age-adjusted median telomere length (95% confidence limit [CI]) among all participants and by the three frailty categories. Median quantile regression was used to examine the association of baseline telomere length with subsequent change in frailty.
Results: At baseline, 131 patients had mean (SD) age of 46.28 (10.16) years, mean disease duration of 15.51 (8.84) years, and mean (SD) SLICC-Damage Index score of 2.24 (2.13). Mean (SD) SLICC-FI score was 0.17 (0.09), with 29.77%, 44.27%, and 25.95% of patients categorized as frail, least fit, and relatively fit respectively. Frail patients had the shortest median telomere length of 3.25 (95% CI 2.43, 4.27) kb, while least fit and relatively fit patients had telomere length of 3.51 (95% CI 2.83, 4.23) kb and 3.35 (95% CI 2.77, 4.97) kb respectively; these differences were not statistically significant (p=0.94). The results were similar after adjusting for baseline age. Baseline telomere length was not associated with median of subsequent change in frailty score (coefficient = 0.0002, 95% CI -0.004, 0.003).
Conclusion: Cross-sectionally, there was not a statistically significant association between telomere length and frailty status. Telomere length was not associated with subsequent change in frailty score in our study, though this may be limited by short follow up time and the small sample size. Further studies are needed to determine the predictive value of telomere length as a biomarker of frailty in lupus patients.
To cite this abstract in AMA style:
Lima K, Legge A, Hanly J, Lee J, Song J, Chung A, Skamra C, Huang Q, Pope R, Ramsey-Goldman R. Association of Telomere Length and the Systemic Lupus International Collaborating Clinics Frailty Index (SLICC-FI) in Long Standing Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/association-of-telomere-length-and-the-systemic-lupus-international-collaborating-clinics-frailty-index-slicc-fi-in-long-standing-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-telomere-length-and-the-systemic-lupus-international-collaborating-clinics-frailty-index-slicc-fi-in-long-standing-systemic-lupus-erythematosus/