Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Cardiovascular complications are increasingly recognized as a significant cause of late mortality in patients with systemic lupus erythematosus (SLE). Although coronary heart disease risk in SLE patients has been extensively studied, the potential risk of heart failure (HF) has received relatively limited attention. This study aimed to comprehensively investigate the incidence and risk of clinically overt HF in a large, population-based, unselected cohort of SLE patients.
Methods: This study employed a retrospective, population-based cohort design using a nationwide insurance database, which covers approximately 99% of the national population, making it one of the most extensive and comprehensive healthcare databases available globally. Utilizing this resource allowed us to substantially minimize selection bias, enabling robust epidemiological research, precise risk factor identification, and accurate outcome assessment. Over a 13-year study period, we identified incident cases of SLE without a prior history of HF. For comparison purposes, non-SLE control groups were selected and matched in a 1:4 ratio to SLE patients based on age, sex, and cohort entry time. The primary outcome was hospitalization due to HF, chosen because hospitalization data provides more accurate diagnosis dates and clearer identification than outpatient records. The cumulative incidence of HF during the follow-up period was estimated using the Kaplan–Meier method. Additionally, multivariable Cox proportional hazards regression analyses were performed to calculate adjusted hazard ratios (HRs) for HF hospitalization, accounting for multiple comorbidities, including diabetes, hypertension, chronic lung disease, chronic kidney disease, dyslipidemia, ischemic heart disease, liver cirrhosis, peripheral vascular disease, and atrial fibrillation.
Results: In total, 7,603 patients with SLE and 30,412 matched controls were included in the analysis. All SLE patients fulfill ACR classification criteria. The mean age of participants after matching was approximately 55 years, with female patients accounting for approximately 75% of the cohort. Hypertension was the most prevalent comorbidity, followed by dyslipid Iemia and diabetes. The cumulative incidence rates of hospitalized HF at 3, 5, and 10 years among SLE patients are illustrated in Figure 1. Compared to non-SLE controls, patients with SLE exhibited a significantly higher risk of developing HF (adjusted HR: 2.47, 95% confidence interval [CI]: 2.12–2.87).
Conclusion: Our findings indicate that SLE is associated with a substantially increased risk of clinically apparent HF, beyond merely asymptomatic ventricular dysfunction. This real-world evidence underscores the importance for rheumatologists to remain vigilant for HF, a potentially fatal complication, in the long-term management and clinical follow-up of patients with SLE.
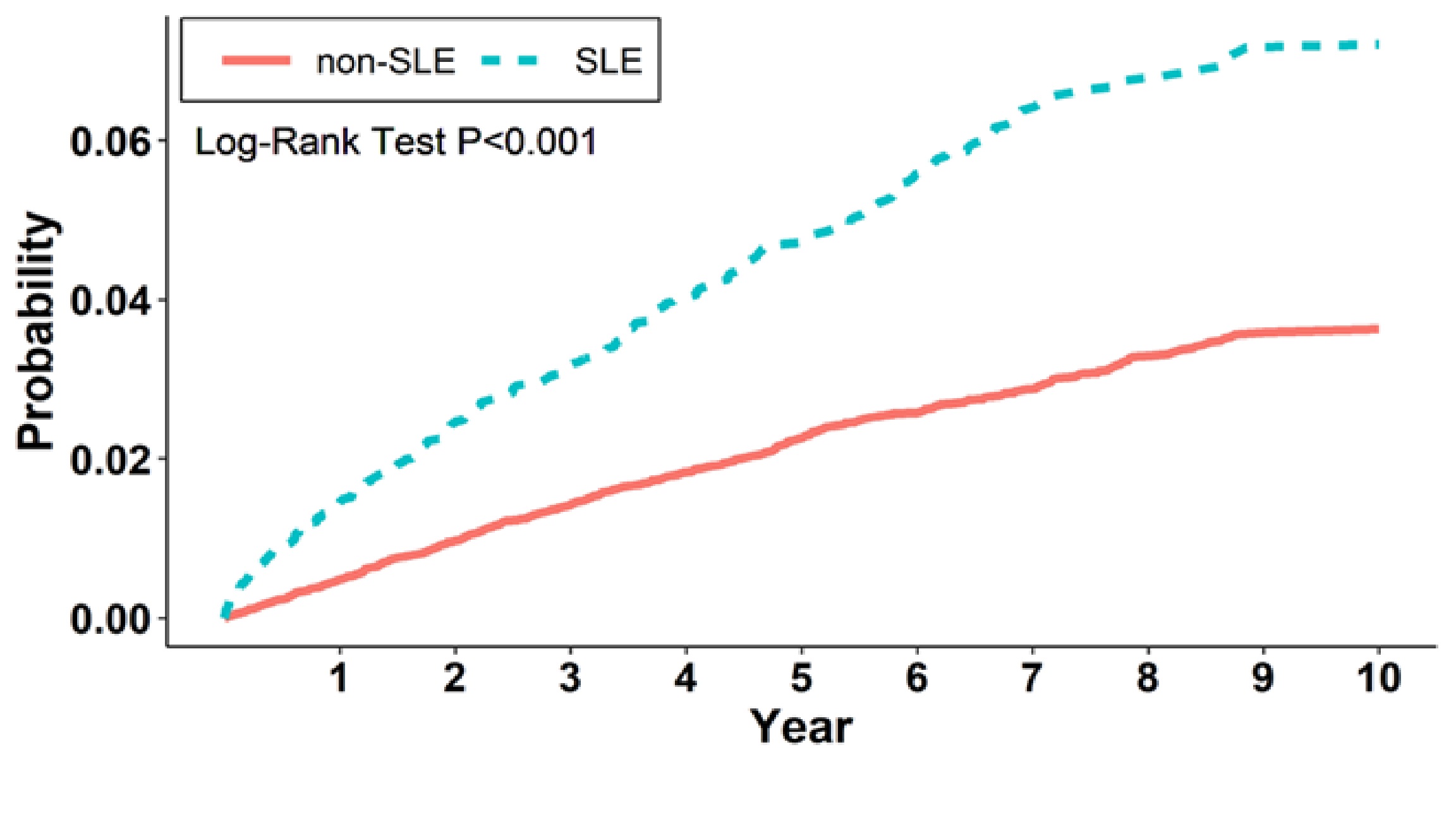 Cumulative incidence of heart failure in SLE patients versus non-SLE patients.
Cumulative incidence of heart failure in SLE patients versus non-SLE patients.
To cite this abstract in AMA style:
Lin C. Association of Systemic Lupus Erythematosus With Incident Heart Failure Requiring Hospitalization [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-of-systemic-lupus-erythematosus-with-incident-heart-failure-requiring-hospitalization/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-systemic-lupus-erythematosus-with-incident-heart-failure-requiring-hospitalization/
