Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Few studies have evaluated clinical outcomes and prognosis of patients with cancer with and without rheumatoid arthritis (RA). Renal cell carcinoma (RCC) is particularly understudied in relation to RA, but evaluation is highly relevant due to standard use of immune checkpoint inhibitors in management. With potential conflicts in the treatment of both RA and RCC, there exists a need to further elucidate outcomes in this unique patient population. Given the adverse outcomes associated with frailty, often present in both conditions, we sought to evaluate all-cause and cancer-specific mortality with a focus on the interactions between frailty, RCC, and RA.
Methods: We collected patient data via the linked Surveillance Epidemiology and End Results cancer registry and Medicare (SEER-Medicare) database. We included non-metastatic patients with the most common subtype of RCC, clear cell Renal Cell Carcinoma (ccRCC), diagnosed from 2004-2017 using ICD-9 and ICD-10 codes. Patients with pre-existing RA were identified if they had ≥2 ICD-9/10 codes for RA within 2 years prior to diagnosis, separately coded 30-365 days apart. Validated Claims-based Frailty (Kim et al 2018) and National Cancer Institute (NCI) Comorbidity indices were extracted within 365 days prior to ccRCC diagnosis. Cox proportional hazards regression models evaluated the association between RA and both all-cause and cancer-specific mortality, adjusting for demographics, socioeconomic status, comorbidities, and cancer stage. For cancer-specific mortality, competing risk analyses were performed and sub-distribution hazard ratios (HR) with 95% confidence intervals (CI) were calculated. Effect modification by frailty status in association with RA and mortality outcomes was assessed.
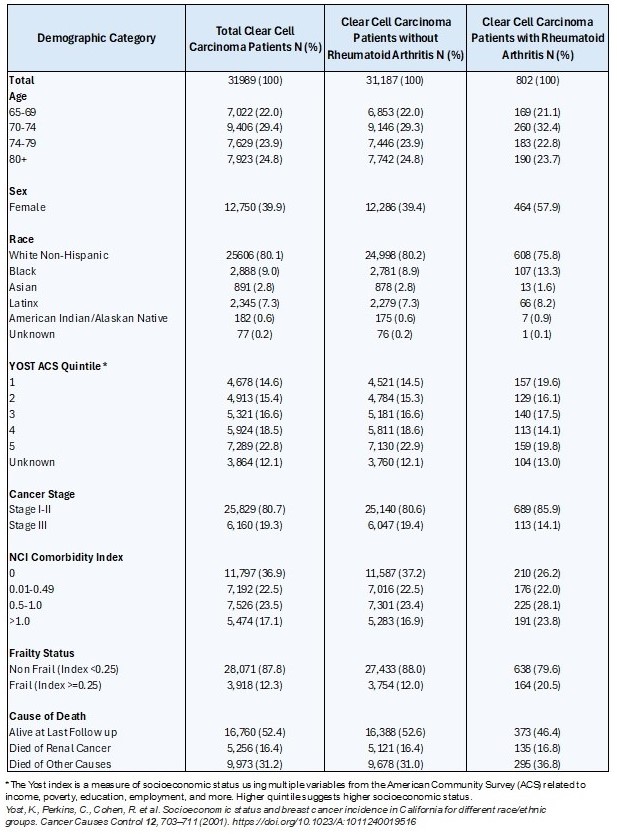
Results: We identified 31,989 patients with non-metastatic ccRCC, of whom 802 (2.5%) had pre-existing RA (Table 1); most had Stage I-II disease (80.7%). Overall, 12.3% met criteria for frailty, including 20.5% of patients with RA vs. 12.0% of patients without RA (p< 0.001).
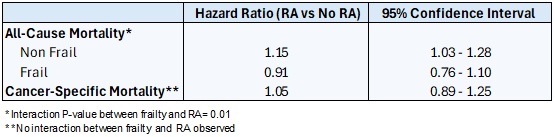
We observed interaction between RA and frailty on all-cause mortality (p = 0.01). The presence of RA in non-frail patients was associated with a significant increased risk of all-cause mortality compared to those without RA (HR 1.15 [95% CI 1.03 – 1.28]). Frail patients with RA (HR 0.91 [95% CI 0.76 – 1.10]), however, did not have a significant difference in all-cause mortality compared to those without RA. No interaction was observed between RA and frailty for cancer-specific mortality (Table 2).
The presence of frailty independently was associated with a significantly increased risk of cancer-specific mortality (HR 1.48 [95% CI 1.36 – 1.61]) while RA was not (HR 1.05 [95% CI 0.88 – 1.25]).
Conclusion: RA was an independent risk factor for all-cause mortality in non-frail patients with non-metastatic ccRCC but not for mortality in frail patients. The presence of frailty, but not RA, was an independent risk factor for cancer specific mortality. Limitations include retrospective nature, selection bias, unmeasured confounders. Our findings are hypothesis-generating and can be used to guide point-of-care discussions in clinic and underscore the importance of further characterizing frailty status.
To cite this abstract in AMA style:
Novin S, Holt S, Swaminathan M, Wright J, Gore J, Hyrich K, Zhao S, Sparks J, Makris U, Suarez-Almazor M, Grivas P, Psutka S, Singh N. Association of Rheumatoid Arthritis and Frailty Status with Mortality in Patients with Renal Cell Carcinoma [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-rheumatoid-arthritis-and-frailty-status-with-mortality-in-patients-with-renal-cell-carcinoma/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-rheumatoid-arthritis-and-frailty-status-with-mortality-in-patients-with-renal-cell-carcinoma/