Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Chronic pain affects 30% of all patients in developed countries, accounting for up to 35% of prescriptions in acute care settings. Non-opioid pain medications are widely utilized for treatment of non-cancer chronic pain. Among these, pregabalin is a commonly prescribed anticonvulsant, which works by antagonizing L-type calcium channels, decreasing the release of neurotransmitters . Pregabalin use has been associated with reports of congestive heart failure (CHF), including peripheral and pulmonary edema. However, the relationship between CHF incidence and pregabalin use among patients at the highest risk of adverse reactions (i.e., senior patients with various co-morbidities) remains unclear. The purpose of this study was to compare incident CHF among new users of pregabalin versus gabapentin (the active comparator) in Medicare beneficiaries treated for non-cancer chronic pain.
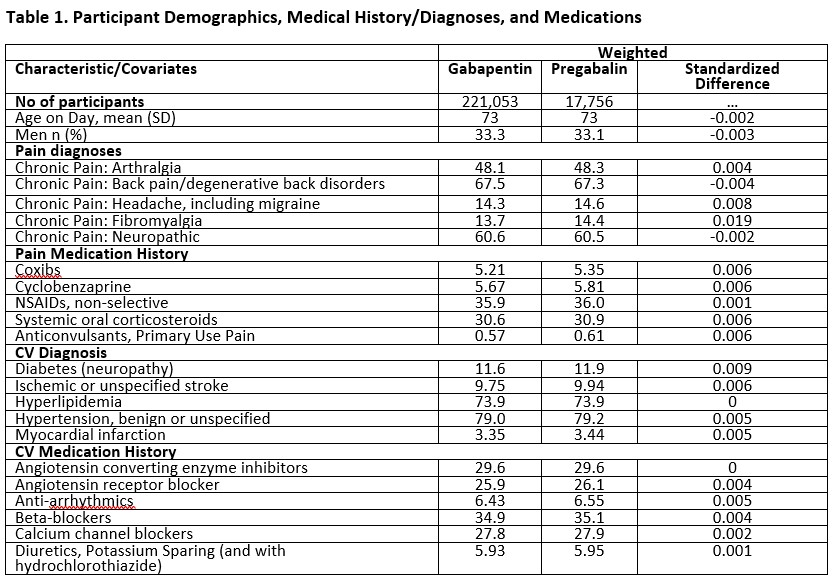
Methods: This was a retrospective cohort study among Medicare beneficiaries aged 65-89 years old with chronic non-cancer pain, without prior history of CHF. Patients who were newly prescribed users of pregabalin or gabapentin were followed up between 2015-2018. The outcome was incident CHF, ascertained by hospital admissions or emergency room visits with ICD 9 and 10 codes in the first position codes. Inverse probability of treatment weighting was used to account for differences between pregabalin and gabapentin users in a time-dependent analysis (i.e., Cox proportional-hazards regressions). A total of 318 covariates were selected for propensity scoring based on prior knowledge and literature review, and included categories such as concurrent baseline cardiovascular, neurologic, pain, and psychiatric diagnoses and corresponding medications including opioids and antipsychotics. Non-diagnostic covariates were included, as well as demographics, socioeconomic status, and indicators/metrics of health care utilization.
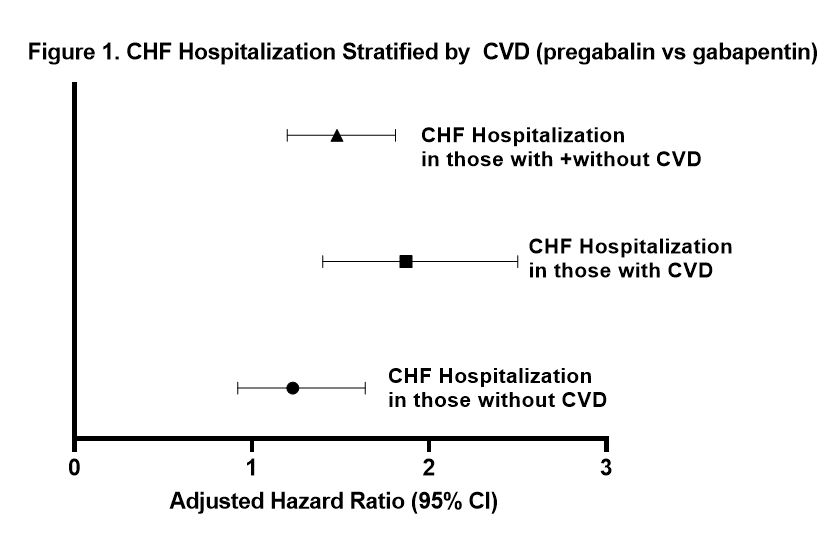
Results: Patient demographics and characteristics are summarized in Table 1. A total of 17,756 new users of pregabalin and 221,053 new users of gabapentin were included. The cohort was predominantly female sex (66.7%) and non-Hispanic White (79.9%), with a median age of 73 years. During 110,439 person-years (PY) of follow-up, 1,428 patients were hospitalized for CHF. The rate for CHF hospitalization was 18.7 per 1000 PY for pregabalin vs 12.6 per 1000 PY for gabapentin (adjusted HR 1.48 (95% CI 1.20-1.81)) (Figure 1). Stratified by cardiovascular disease (CVD), the rate of CHF hospitalization was 42.9 for pregabalin vs 23.4 for gabapentin (adjusted HR 1.87 (95% CI 1.40-2.60)) (Figure 1).
Conclusion: In this retrospective study of Medicare beneficiaries aged 65-89 years with chronic non-cancer pain, new users of pregabalin had higher rates of incident CHF hospitalizations or emergency room visits compared to new users of gabapentin.
To cite this abstract in AMA style:
Park E, Daniel L, Dickson A, Corriere M, Nepal P, Hall K, Plummer D, Dupont W, Murray K, Stein C, Ray W, Chung C. Association of Pregabalin vs Gabapentin with Incident Congestive Heart Failure in Patients with Non-Cancer Pain [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-of-pregabalin-vs-gabapentin-with-incident-congestive-heart-failure-in-patients-with-non-cancer-pain/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-pregabalin-vs-gabapentin-with-incident-congestive-heart-failure-in-patients-with-non-cancer-pain/