Session Information
Date: Sunday, November 7, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Manifestations (0855–0896)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Cognitive dysfunction (CD) is a common manifestation of systemic lupus erythematosus (SLE) which can have detrimental consequences for those affected. To date, no treatments have been approved for SLE-associated CD (SLE-CD). This study aims to assess the association of azathioprine (AZA) and mycophenolate (MMF) use with SLE-CD, given that these medications have demonstrated neuroprotective qualities in prior studies.
Methods: Consecutive adult SLE patients presenting to a single center were screened. The American College of Rheumatology (ACR) neuropsychological battery (NB) for SLE, evaluating 6 cognitive domains, was administered to consenting participants at 0, 6 and 12 months. Age and gender matched normative data were used to obtain z-scores. CD was determined by a z-score of £-1.5 in ³2 cognitive domains. Non-CD was defined as no z-score £-1.5. MMF and AZA use were recorded as cumulative dose (grams per kilogram [g/kg]), duration of treatment (number of years) and current use for ³6 months from visit day. Clinical and demographic characteristics were verified at each visit. Baseline characteristics by cognitive status and medication use were documented. Mixed-effects logistic regression models were constructed to estimate the odds of CD and non-CD with respect to AZA and MMF use over the three follow-up periods.
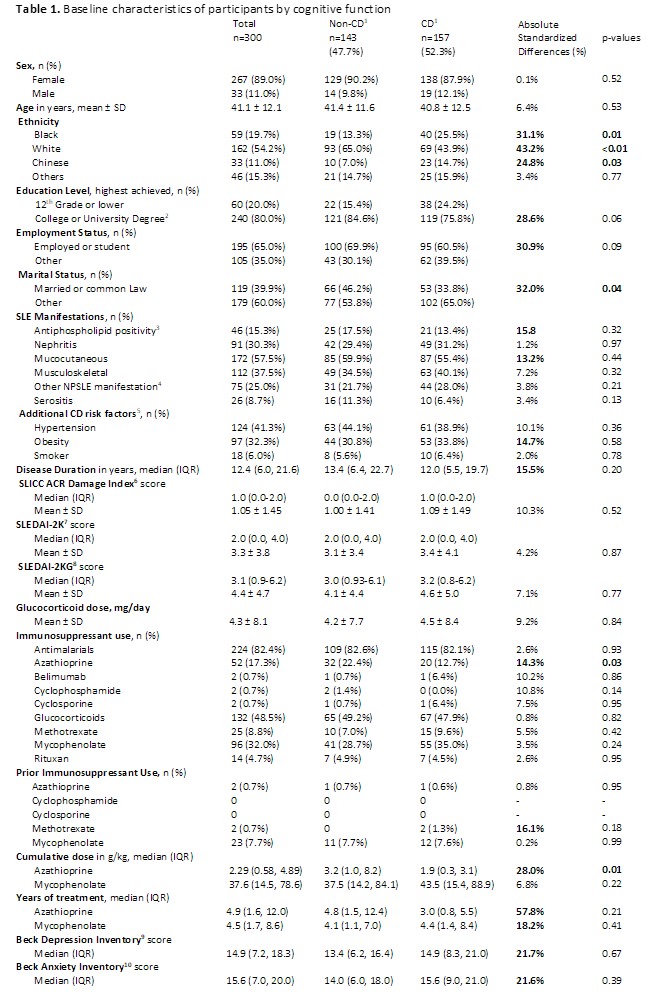
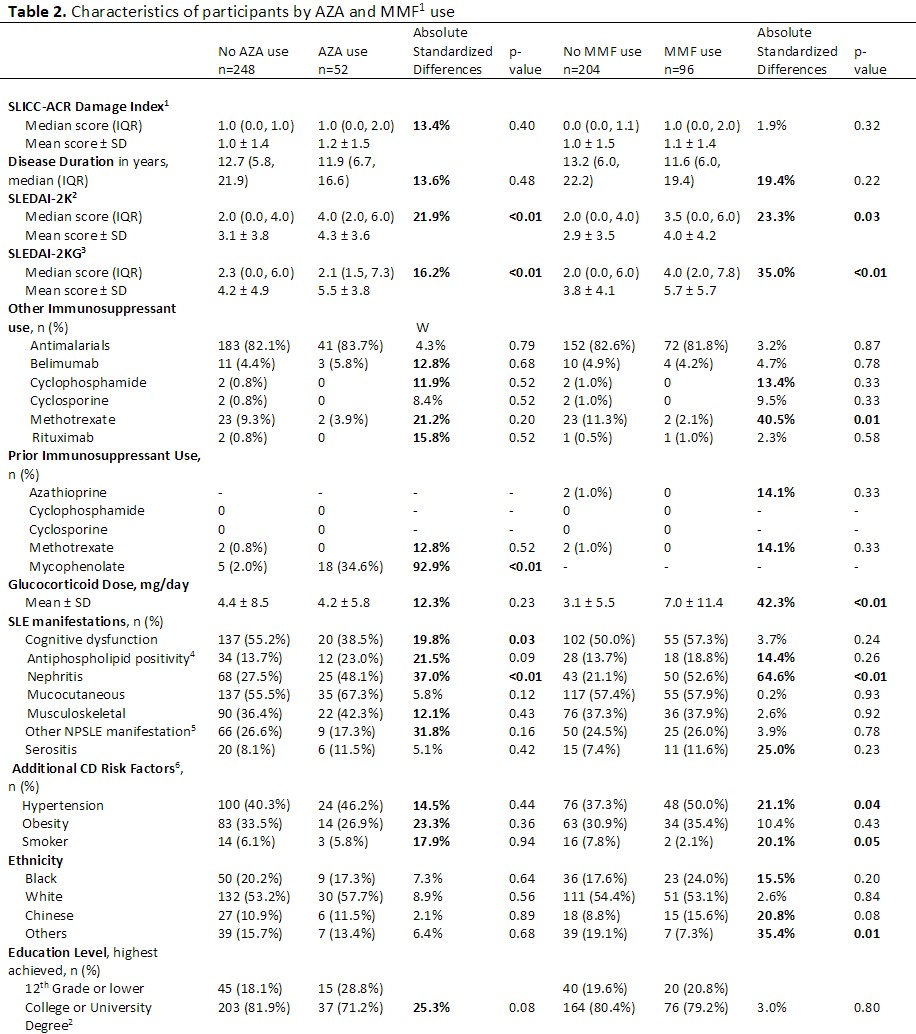
Results: Three hundred participants representing 676 patient visits completed the study; 157 (52%) met criteria for CD at baseline. Mean age was 41.1 years (SD 12.1) and 267 participants (89.0%) were female. Table 1 outlines baseline characteristics by CD and non-CD status. There were no significant differences in mean age, glucocorticoid dose, disease duration, SLE Disease Activity Index-2000 (SLEDAI-2K) scores, or SLICC-ACR Damage Index (SDI) scores. In contrast, there were significantly more participants with CD who identified as Black or Chinese, and significantly fewer participants identifying as White. There were also fewer married participants with CD. Table 2 documents baseline characteristics by AZA and MMF use with respect to CD status. Participants taking AZA or MMF had significantly higher SLEDAI-2K scores and higher prevalence of nephritis; participants taking MMF had higher rates of hypertension, higher daily doses of glucocorticoid medications and lower rates of smoking.
Table 3 shows results of the mixed effects models for AZA and MMF use versus CD. For each g/kg of cumulative AZA, there was on average a 24% reduced odds of CD: OR 0.76, 95% CI 0.61, 0.96, p=0.02. For each year of AZA treatment there was on average a 32% reduced odds of CD: OR 0.68 (0.50, 0.94), p=0.02. AZA use as binary variable (yes versus no) demonstrated a consistent trend toward reduced odds of CD with AZA use without reaching statistical significance: OR 0.29 (0.08, 1.12), p=0.07. Cumulative AZA dose was not significantly associated with non-CD status: 1.08 (0.91, 1.27), p=0.38 (not shown). MMF use was not associated with CD or non-CD.
Conclusion: Despite higher disease activity scores in participants taking AZA compared to those not taking AZA, cumulative AZA dose and increasing AZA treatment duration were associated with significantly lower odds of SLE-CD. MMF use was not associated with SLE-CD.
2) Completion of post-secondary schooling including a College (≥2 years) or University (≥4 years) degree.
3) Positive lupus anticoagulant testing, and/or anti-beta2glycoprotein1 IgG or IgM, and/or anti-cardiolipin IgG or IgM above laboratory specific upper limit of normal, at baseline and again after ≥12 weeks.
4) Psychosis, seizures, stroke, neuropathy and/or transverse myelitis.
5) Known risk factors for cognitive dysfunction not captured elsewhere.
6) SLICC ACR: Systemic Lupus International Collaborating Clinics / American College of Rheumatology Damage Index.
7) SLEDAI_2K: Systemic Lupus Erythematosus Disease Activity Index 2000.
8) SLEDAI_2KG: Systemic Lupus Erythematosus Disease Activity Index 2000 Glucocorticoid Index.
9) Beck Depression Inventory score of 0–13 is considered minimal, 14–19 mild, 20–28 moderate and 29–63 severe.
10) Beck Anxiety Inventory score of 0-7 is considered minimal, 8_15 mild, 16_25 moderate and 26-63 severe.
1) SLICC-ACR DI: Systemic Lupus International Collaborating Clinics American College of Rheumatology Damage Index.
2) SLEDAI_2K: Systemic Lupus Erythematosus Disease Activity Index 2000.
3) SLEDAI_2KG: Systemic Lupus Erythematosus Disease Activity Index 2K Glucocorticoid.
4) Positive lupus anticoagulant testing, and/or anti-beta2glycoprotein1 IgG or IgM, and/or anti-cardiolipin IgG or IgM above laboratory specific upper limit of normal, at baseline and again after ≥12 weeks
5) Psychosis, seizures, stroke, neuropathy and/or transverse myelitis.
6) Known risk factors for cognitive dysfunction not captured elsewhere.
OR: odds ratio; CI: confidence interval.
Covariates included in the models: Systemic Lupus Erythematosus Disease Activity Index_2000 Glucocorticoid (SLEDAI_2KG) score (incorporates glucocorticoid dose with the SLE Disease Activity Index 2000 [SLEDAI_2K]), Systemic Lupus International Collaborating Clinics (SLICC) – American College of Rheumatology (ACR) Damage Index score (SDI), additional CD risk factors not captured elsewhere (hypertension, obesity, active smoker), persistent antiphospholipid antibody positivity (positive lupus anticoagulant testing, and/or anti-beta2glycoprotein1 IgG or IgM, and/or anti-cardiolipin IgG or IgM above laboratory specific upper limit of normal, at baseline and again after ≥12 weeks, recorded as binary variable), history of lupus nephritis, active use of an additional immunomodulator (antimalarials, belimumab, calcineurin inhibitor, cyclophosphamide, methotrexate, rituximab), prior use of an immunomodulator (AZA, calcineurin inhibitor, cyclophosphamide, methotrexate, MMF), Beck Depression Inventory (BDI) scores, Beck Anxiety Inventory (BAI) scores, age in years, sex (male versus female), ethnicity (Black, Caucasian, Chinese or other), education level (completion of a College or University degree recorded as binary variable), employment status (employed or full time student versus other) and marital status (married or common-law partner versus other).
To cite this abstract in AMA style:
Dobrowolski C, Su J, McGinley J, Fazzari M, Bingham K, Anderson N, Beaton D, Ruttan L, Wither J, Tartaglia M, Kakvan M, Bonilla D, Choi M, Fritzler M, Katz P, Green R, Putterman C, Touma Z. Association of Mycophenolate and Azathioprine Use with Cognitive Function in SLE [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-mycophenolate-and-azathioprine-use-with-cognitive-function-in-sle/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-mycophenolate-and-azathioprine-use-with-cognitive-function-in-sle/