Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Antiphospholipid antibody (aPL) positivity is associated with elevated risk of thrombosis among patients with SLE, but other clinical associations are less well-known. The goal of our study was to determine clinical correlations with aPL seropositivity among patients with SLE to help inform risk factor prediction models and provide insights to improve management strategies.
Methods: We used data from a longitudinal research registry of patients with SLE seen at our institution between 2003-2020. Patients were selected using a case-control design based on having known aPL and/or lupus anticoagulant (LAC) status (normal or elevated). aPL status included IgM and IgG anticardiolipin and anti-b2glycoprotein, categorized by Ig level (any positive >20 GLP/MLP, or high positive >40 GLP/MLP). Demographic information, American College of Rheumatology (ACR) and SLICC classification criteria for SLE, SLICC Damage Index (SDI), and renal biopsies were evaluated. Statistical analysis was performed using Fisher’s exact or Pearson’s chi-squared testing.
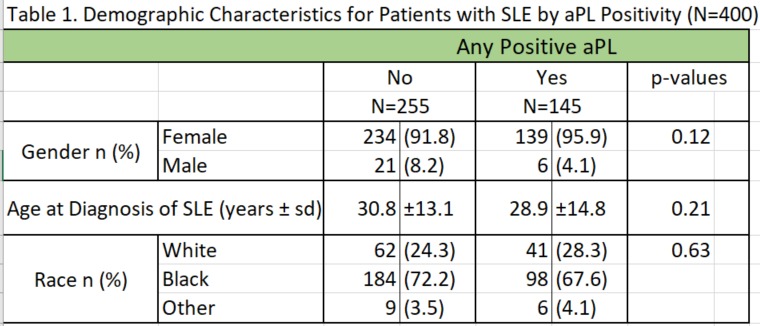
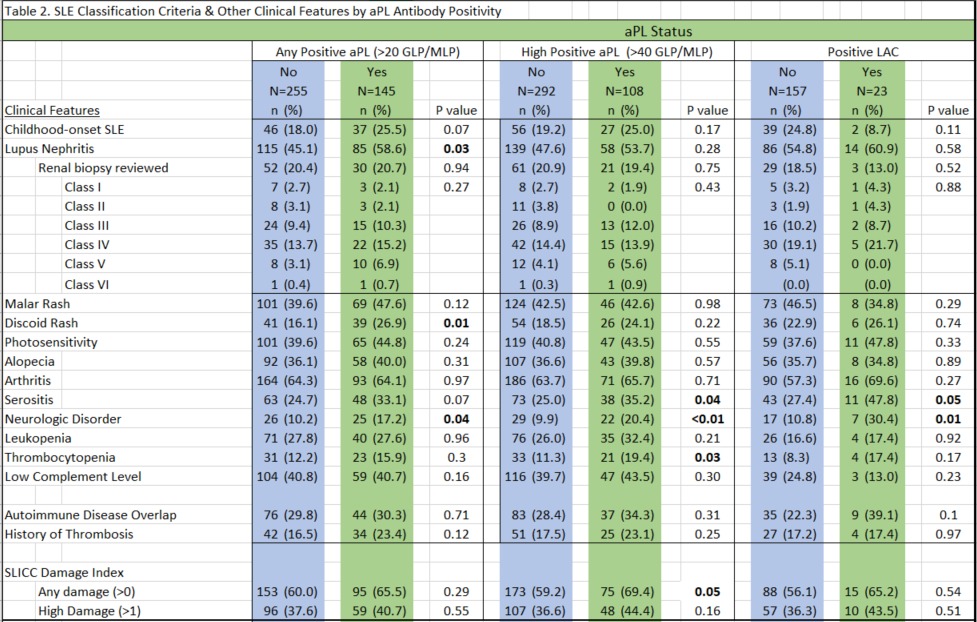
Results: A total of 400 patients with SLE were evaluated, the majority black (69.9%) and female (93.9%). Table 1 compares aPL status by race, gender, and age of SLE diagnosis. Table 2 compares aPL and LAC status by presence of clinical characteristics. Lupus nephritis was more prevalent among black compared to non-black patients (59.3% vs. 26.4%, p< 0.01), childhood-onset SLE compared to those diagnosed in adulthood (67.1% vs. 45.8%, p< 0.01), and men compared to women (64.7% vs. 48.9%, p=0.07). Table 2 shows associations between clinical characteristics and any positive aPL, high positive aPL, and positive LAC. Positive aPL was associated with lupus nephritis in 58.6% of patients compared to 45.1% of those negative for aPL (p=0.03). After evaluating renal biopsy data, we found no significant difference in nephritis biopsy classes between those positive or negative for aPL or LAC. In addition to nephritis, discoid rash and neurologic disorder were significantly associated with positive aPL status. Serositis, thrombocytopenia and neurologic disorder were significantly associated with high positive aPL and neurologic disorder with positive LAC. High positive aPL was associated with disease damage, as measured by SDI, but no significant difference was seen with lower titer positive aPL or LAC positivity. Although no significant difference was seen in prevalence of thrombosis and aPL status, the use of low dose aspirin (45.5%) and warfarin (18.6%) were significantly higher among patients with any positive aPL compared to those negative for aPL (p< 0.01).
Conclusion: We found that within this predominately African American cohort of patients with SLE, elevated levels of aPL antibodies are associated with lupus nephritis, discoid rashes, and neurologic disorder. At high titers, aPL status was associated with serositis, neurologic disorder and thrombocytopenia. The strongest association of LAC was with neurologic disorder. Further studies will determine the timing of aPL status to these clinical manifestations and potential benefit of antiplatelet and/or anticoagulation on nonthrombotic manifestations such as lupus nephritis, when aPL antibodies are elevated.
To cite this abstract in AMA style:
Jain P, Oates J, Wilson D, Kamen D. Association of Lupus Nephritis and Other Clinical Features with Antiphospholipid Antibody Positivity Among Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-lupus-nephritis-and-other-clinical-features-with-antiphospholipid-antibody-positivity-among-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-lupus-nephritis-and-other-clinical-features-with-antiphospholipid-antibody-positivity-among-patients-with-systemic-lupus-erythematosus/