Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Glucocorticoids (GCs) have long been a mainstay of treatment for SLE. While GCs do provide benefit, there are potential side effects that increase with dose and duration and that have potential to affect quality of life negatively. In these analyses, we examine the association of GC use and patient-reported outcomes (PROs).
Methods: Data are from the FORWARD Databank questionnaires collected from participants with physician-diagnosed SLE at 6-month intervals from July 2015 – July 2020.Respondents provide comprehensive health information including GC use and dosage during the prior 6 months and complete PROs, including PROMIS Physical Function, Fatigue, Pain Interference, Sleep Disturbance, and Satisfaction with Social Roles; Systemic Lupus Activity Questionnaire (SLAQ); PHQ-8 (depressive symptoms); and a numeric rating scale of pain (0–10).Analyses examined PROs at baseline according to GC use/non-use. For GC users, baseline data were drawn from the questionnaire in which GCs were first reported during the analysis period. For non-users, baseline data were drawn from the first questionnaire completed during the observation period. Longitudinal logistic regression analyses used generalized estimating equation (GEE) models to estimate the likelihood of worsening in PROs from prior to current observation (by ≥0.5 standard deviation) based on increases in GC dose, addition of other medications, or both during the same period. Models controlled for age, sex, race, BMI, comorbidities, education level, smoking, SLE duration, self-reported lupus disease activity, and SLE organ damage measured by BILD (Brief Index of Lupus Damage).
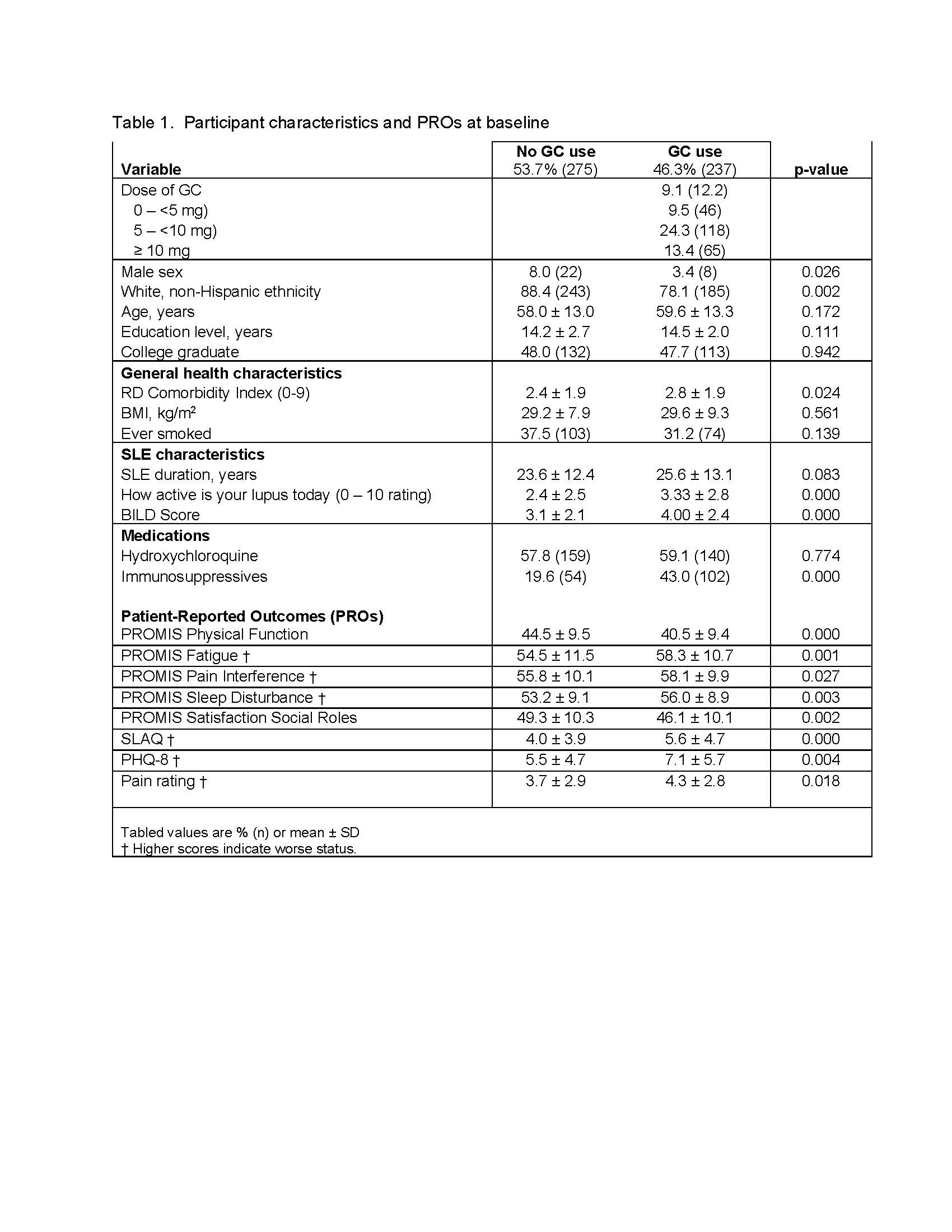
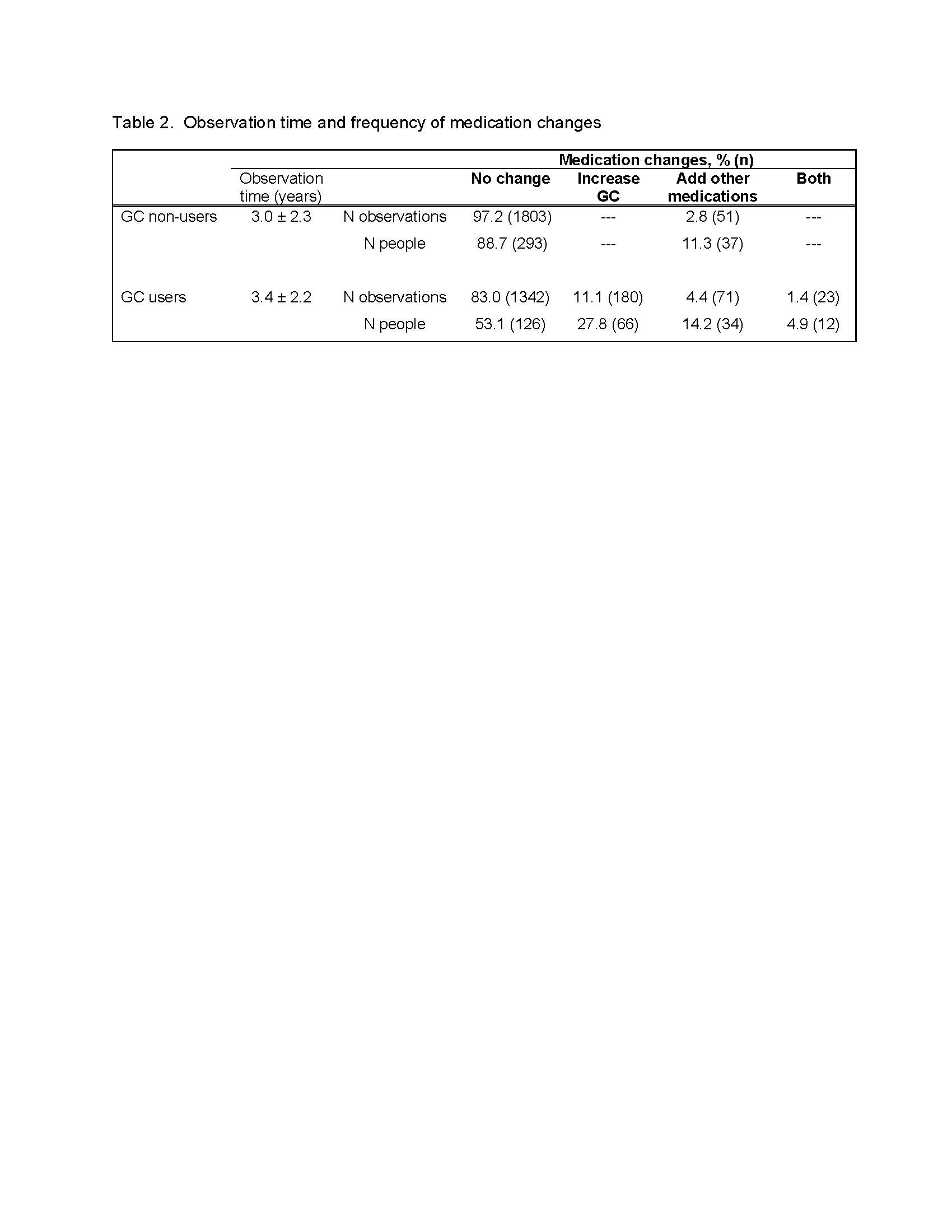
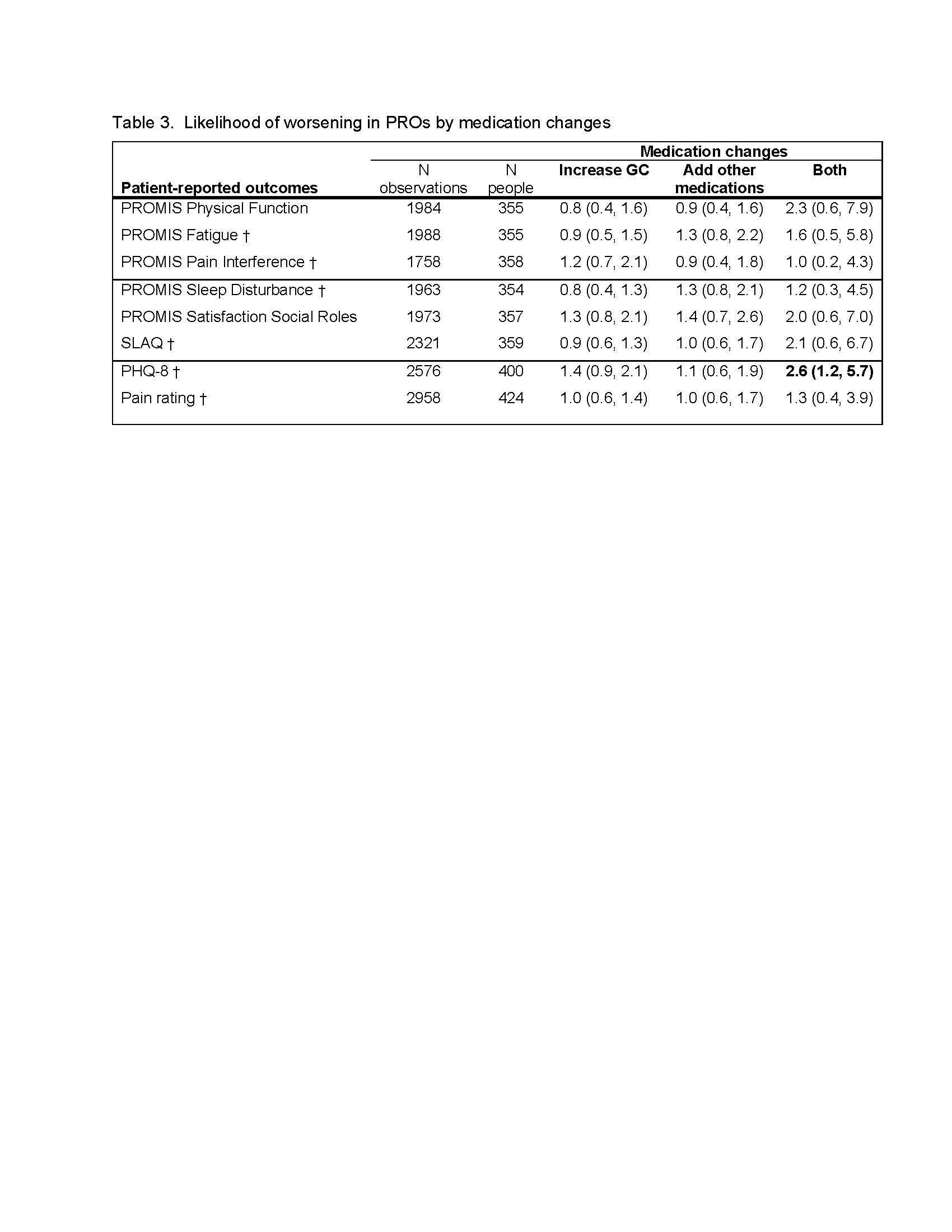
Results: 512 participants qualified for the analysis; 46.3% reported GC use in at least one 6-month period (Table 1).GC users were less likely to be male or white, had more comorbidities, had longer SLE duration, were more likely to also be taking immunosuppressive medications, and reported more active SLE and greater disease damage. GC users had worse scores on all PROs at baseline (Table 1).Non-GC users rarely had medication changes (97% of observations, 89% of GC non-users; Table 2). The majority of GC users also had no medication changes (83% of observations, 53% of GC users). However, increases in GC dose were noted in 11.1% of observations, other medications added in 4.4%, and both GC increases and medication additions in 1.4%.Increases in GC dose, addition of other medications, or the combination were not associated with PRO worsening (Table 3).The exception was PHQ, for which there was a significant likelihood of higher scores in the group with increase in GC plus addition of another medication.
Conclusion: GC use was associated worse with PROs at the baseline for these analyses. In this non-inception cohort with relatively long disease duration, however, PROs generally did not worsen over time with changes in GC dosage or other medications; i.e., the differences between GC users and non-users appeared to be static over time. Results suggest that despite potential side effects, patients tend to remain on relatively stable GC doses over time. Patients may be willing to risk negative side effects of GCs to avoid further worsening of symptoms such as pain and fatigue.
To cite this abstract in AMA style:
Katz P, Pedro S, Choi J, Michaud K. Association of Glucocorticoid Use with Patient-Reported Outcomes Among Persons with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/association-of-glucocorticoid-use-with-patient-reported-outcomes-among-persons-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-glucocorticoid-use-with-patient-reported-outcomes-among-persons-with-systemic-lupus-erythematosus/