Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: The Idiopathic inflammatory myopathies are a heterogeneous group of rare systemic autoimmune diseases with muscle as the primary target. Fatigue is one of the most common and prominent symptoms reported by myositis patients. Activities of daily living are frequently affected by fatigue. In this study, we investigated the cross-sectional and longitudinal association of fatigue in myositis with established clinical outcome measures.
Methods: Myositis patients [Dermatomyositis (DM), necrotizing myopathy (NM), Polymyositis(PM), and anti-synthetase syndrome (AS)] evaluated at the University of Pittsburgh Myositis Center were prospectively enrolled. Patients with active disease (defined as the escalation of immunosuppressive therapy in the previous 6 months) and inactive disease were assessed at 0, 3, and 6 months. At each of these visits, myositis core set measures (CSMs) [muscle enzymes, manual muscle testing (MMT), patient and physician global disease activity, extra-muscular disease activity, and HAQ], task-oriented functional measures [Timed up and go (TUG), Sit to Stand (STS), 6 Minute Walk Distance (6-MWD)], and patient-reported outcomes [Patient-Reported Outcomes Measurement Information System-physical function (PROMIS-PF), Short Form- 36 (SF-36) physical and mental component summary (PCS, MCS)] were evaluated. Fatigue was evaluated using the vitality domain (energy/fatigue) of the SF-36 and a 10 cm Visual Analog Scale (VAS) for fatigue (mild 0-3; moderate 3-7; severe 7-10). The phenotypic and disease activity measures of the cohort were correlated with fatigue measures using Spearman at the baseline visit. Longitudinal changes were associated with clinical improvement (per 2016 ACR/EULAR myositis response criteria) as well as physician and patient global assessment of change using the Chi-square test.
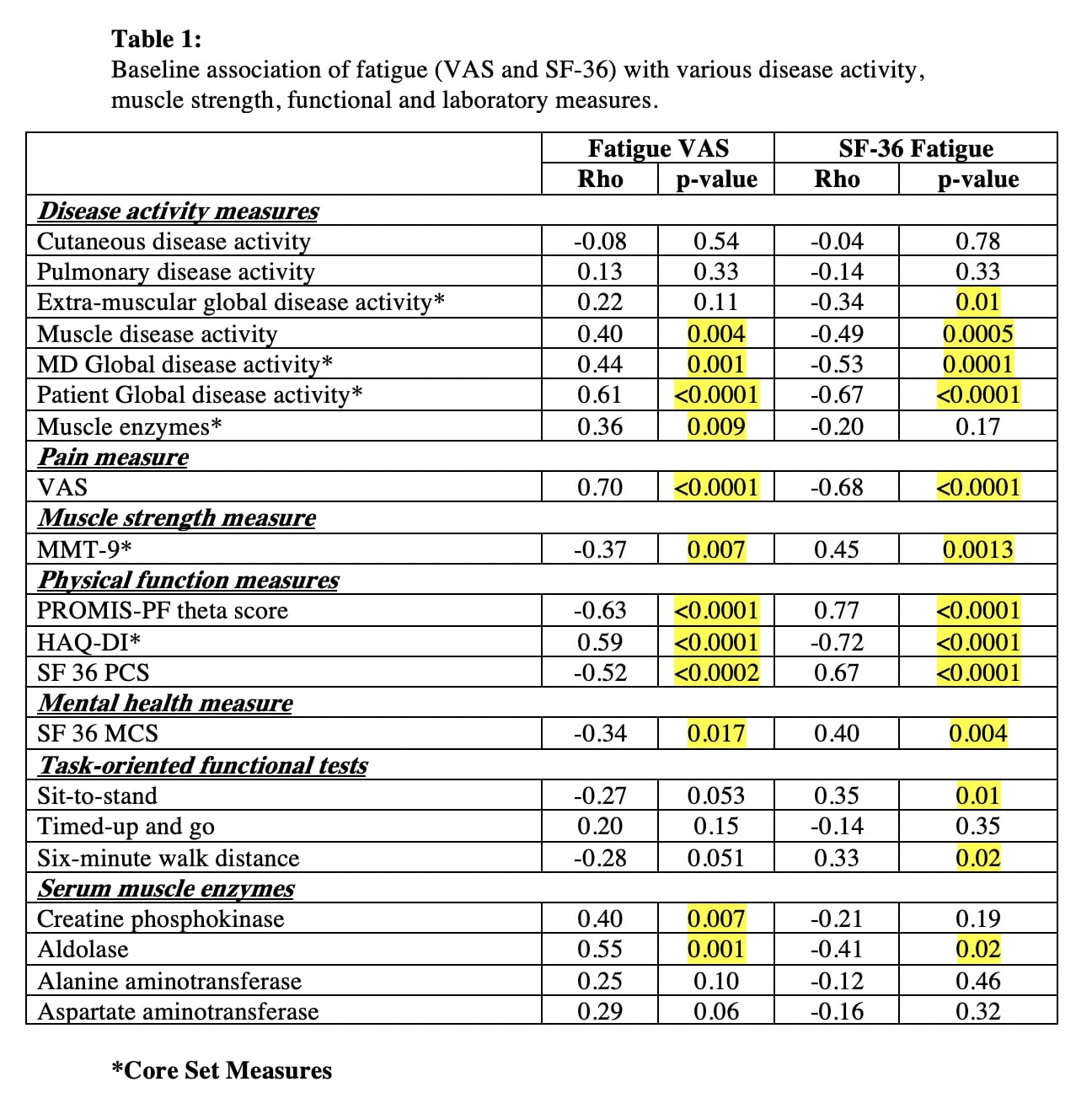
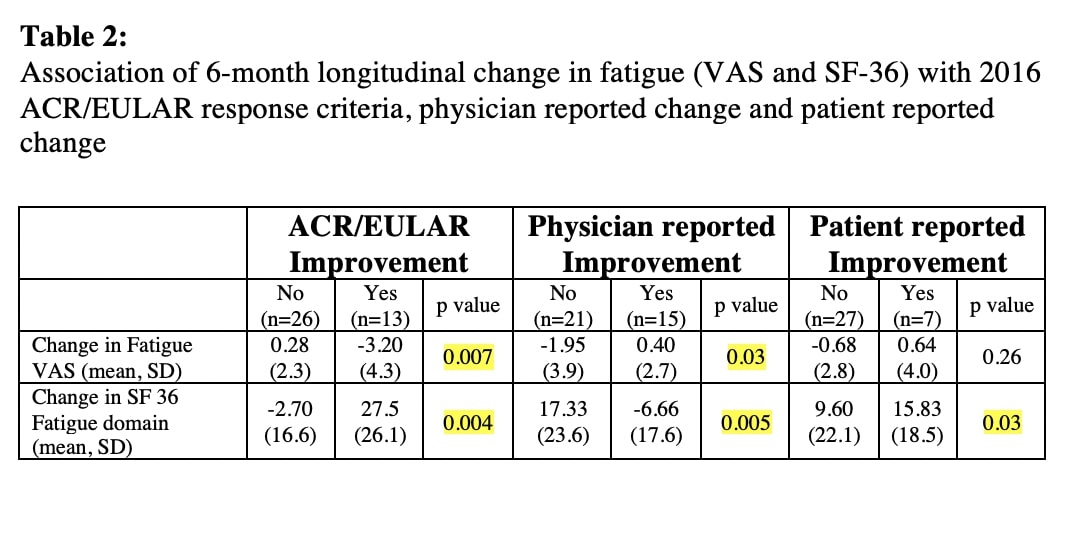
Results: Fifty patients [mean age, 51.6 (±14.9); 60% females] were studied: 6 PM, 24 DM, 9 NM, and 11 AS (without clinical myositis). The mean (SD) severity of fatigue (0-10) was 4.2 (3), with most patients having moderate (51%) or severe (16%) fatigue at baseline. No difference was observed with respect to gender, disease subtypes (DM, non-DM), or age at enrollment. However, at baseline, fatigue (both VAS and SF-36 domain) was significantly associated with active myositis and having muscle weakness. Fatigue measures showed moderate to strong correlation with several myositis disease activity measures including CSMs, pain, and patient-reported outcomes of physical function (table 1). Physical function measures such as PROMIS-PF, HAQ-DI, SF-36 PCS, and MCS also had a statistically strong correlation with fatigue. The longitudinal analysis over the 6-month study period suggested that fatigue improved significantly with improvement in myositis disease activity as assessed by 2016 ACR/EULAR response criteria as well as physician and patient-reported assessment of change in disease activity.
Conclusion: Fatigue is common in myositis and has a moderate to strong correlation with disease activity measures, muscle strength, and functional outcome measures. Further, an improvement in fatigue is associated with the clinical response using the ACR/EULAR myositis response criteria.
To cite this abstract in AMA style:
Bijoy George T, Chandrasekhara Pillai A, Moghadam-Kia S, Neiman N, Ascherman D, Oddis C, Ren D, Aggarwal R. Association of Fatigue with Disease Activity in Myositis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-fatigue-with-disease-activity-in-myositis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-fatigue-with-disease-activity-in-myositis/