Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Sjogren’s syndrome (SS) is a heterogenous systemic inflammatory autoimmune disease characterized by sicca symptoms. It affects 0.3-1 per 1000 of the general population1. Studies suggest that novel autoantibodies or “early Sjögren’s syndrome markers,” particularly salivary protein 1 (SP1), carbonic anhydrase 6 (CA6), and parotid specific protein (PSP) are present in early disease, prior to anti-Ro and anti-La positivity. We aimed to define the usefulness of these early markers as they relate to diagnosis, risk stratification, and presence of disease associations.
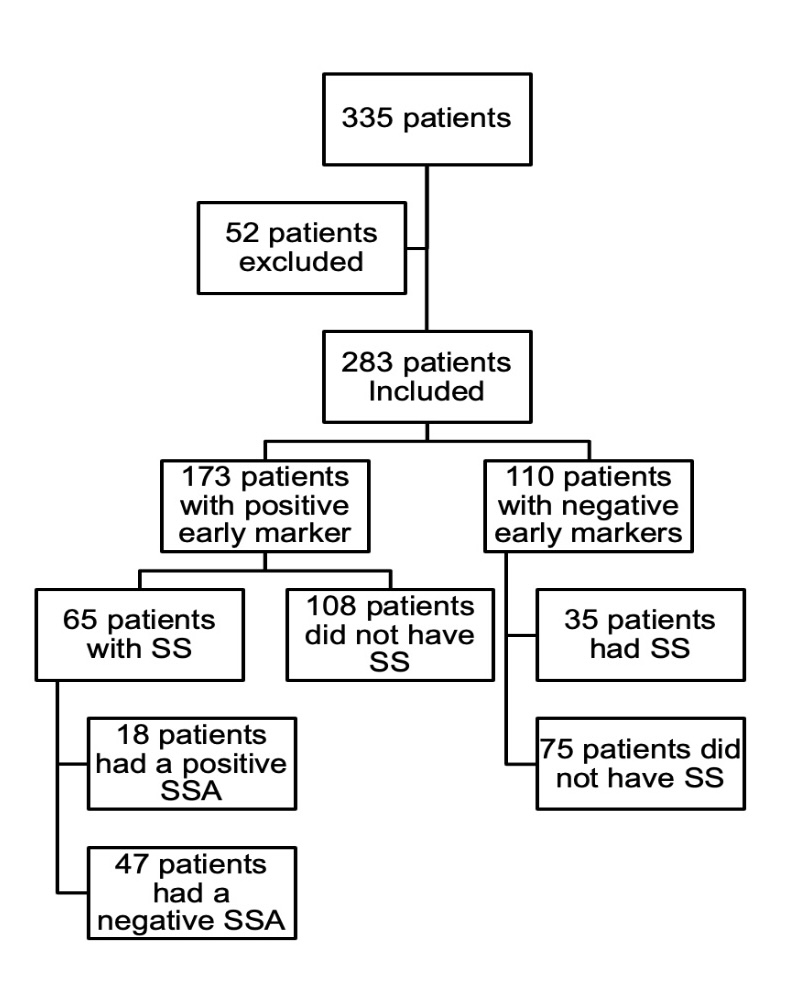
Methods: This retrospective study included 335 patients with SS and sicca symptoms specific ICD-10 codes: M35.00, M35.01, H16.209, H04.129, H04.123, R68.02. Patients also had early Sjögren’s markers ordered between 01/01/2017 to 12/31/2022. Patients with sicca symptoms associated with Hepatitis C, AIDS, Sarcoidosis, or head and/or neck radiation were excluded. Early Sjogren’s antibody positivity was defined as having a reported value ≥ 25 EU/ml, which is considered strongly positive across various laboratories. Chi-square test of independence was used to analyze the results for statistical significance.
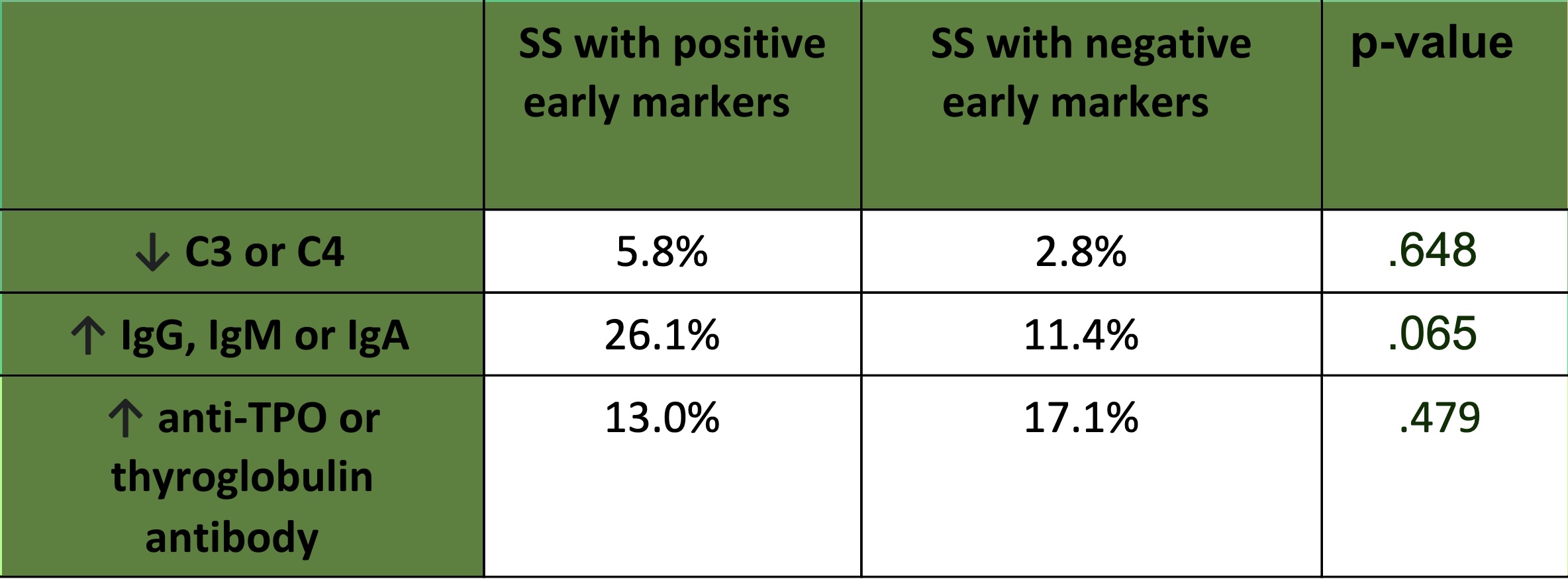
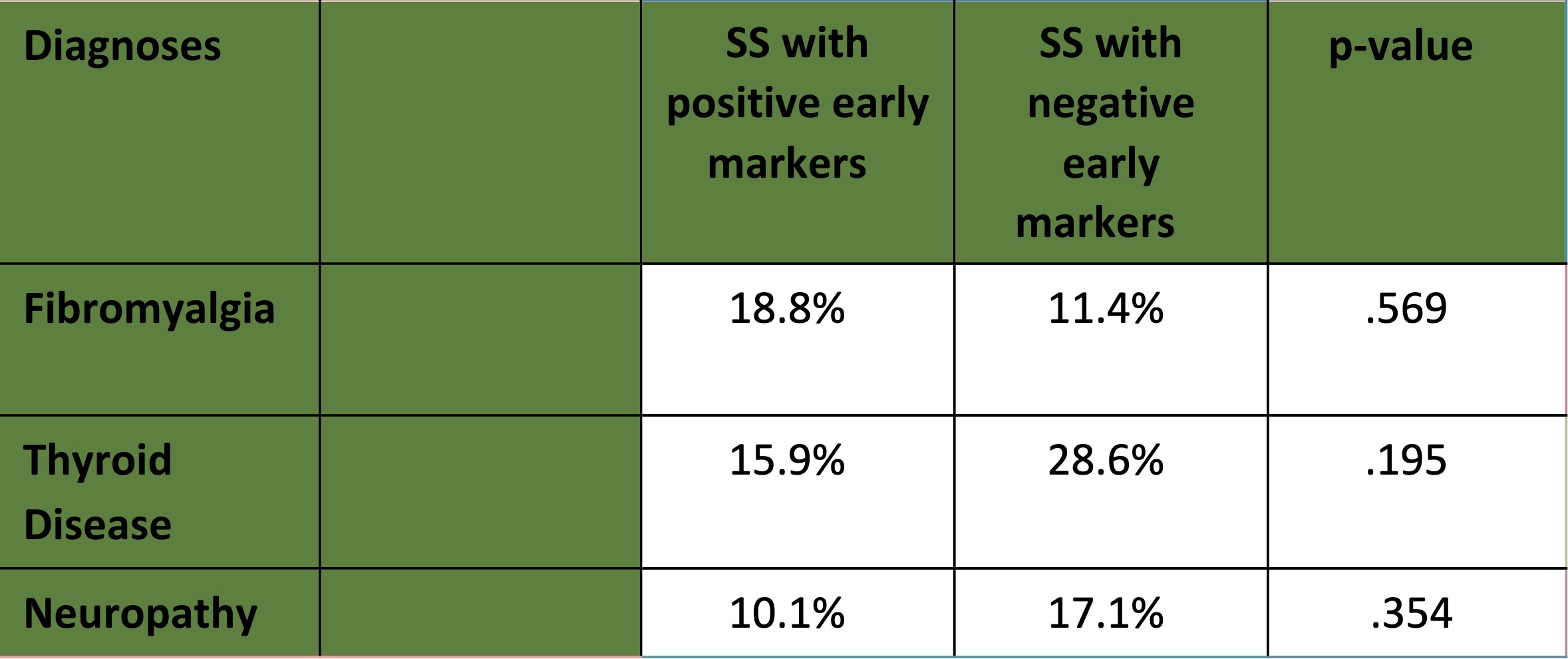
Results: Two hundred and eighty-three patients were included of which greater than 50% were identified as being Hispanic/Latino as reported by medical records. We found positive early antibodies present in 54.9% (95 patients) of Hispanic/Latino ethnicity, 39.9% (69 patients) non-Hispanic/Latino, and 5.2% (9 patients) other. Sixty-one percent of patients were positive for one or more early Sjögren’s markers. In patients with positive early Sjögren’s markers, 37.5% had a clinical diagnosis of SS, and 11% had a diagnosis of a rheumatic connective tissue disease (CTD) other than SS. Of the remaining 51.5% who did not have a CTD, 81% had sicca symptoms. Of patients with SS, 30% of those with positive early markers were SSA antibody positive. There was no statistically significant association between early Sjögren’s markers and a diagnosis of SS, X2 (1, N = 283) = 1.8, p = .35. In patients with SS with at least one positive marker: 19% had fibromyalgia, 16% had thyroid disease, 10% had peripheral neuropathy. Patients with SS with positive early markers were found more likely to have hypocomplementemia and hypergammaglobulinemia when compared to patients with SS without positive early markers. However, this finding did not reach statistical significance. Anti-CA6 was the most prevalent antibody in patients with and without a diagnosis of SS.
Conclusion: In this diverse cohort of patients, there was no statistically significant association between early Sjögren’s markers, and a diagnosis of SS. Findings suggest that these antibodies may not be disease specific. In patients with disease associated manifestations, early Sjögren’s antibody positivity was small. Prospective longitudinal studies of interest would include phenotyping SS patients with early markers as a determinant of disease.
Karakus, S., Baer, A. N., Agrawal, D., Gurakar, M., Massof, R. W., & Akpek, E. K. (2018). Utility of novel autoantibodies in the diagnosis of sjögren’s syndrome among patients with dry eye. Cornea, 37(4), 405–411. doi:10.1097/ico.0000000000001471
To cite this abstract in AMA style:
Henry D, Culpepper Pace S. Association of Early Markers in Patients with Sjögren’s Syndrome in a Diverse Academic Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-of-early-markers-in-patients-with-sjogrens-syndrome-in-a-diverse-academic-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-early-markers-in-patients-with-sjogrens-syndrome-in-a-diverse-academic-cohort/