Session Information
Date: Saturday, November 6, 2021
Title: Epidemiology & Public Health Poster I: COVID-19 & Vaccination (0084–0117)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Patients with immune-mediated diseases have similar risk of severe COVID-19 versus the general population but CD20 inhibitor users may be at increased risk of COVID-19-related death. We examined whether CD20 inhibitor users have worse COVID-19 outcomes than general population comparators.
Methods: We performed a comparative cohort study of CD20 inhibitor users in immune-mediated diseases and general population comparators for COVID-19 outcomes. We identified cases who used CD20 inhibitors for immune-mediated diseases (non-oncologic/non-transplant indication) within one year prior to index date of PCR-confirmed COVID-19 between January 31, 2020, and January 31, 2021, in a large healthcare system. Details regarding demographics, medical history, CD20 inhibitor treatment, and COVID-19 were extracted from the electronic health record. Comparators with COVID-19 were matched up to 5:1 by age, sex, and index date of PCR positivity. We estimated hazard ratios (HRs) and 95% confidence intervals (CIs) for hospitalization, mechanical ventilation, and death in CD20 inhibitor users versus comparators using Cox regression. We also assessed these associations among cases with rheumatic conditions and shorter (< 1 year) or longer ( >1 year) CD20 inhibitor duration versus comparators.
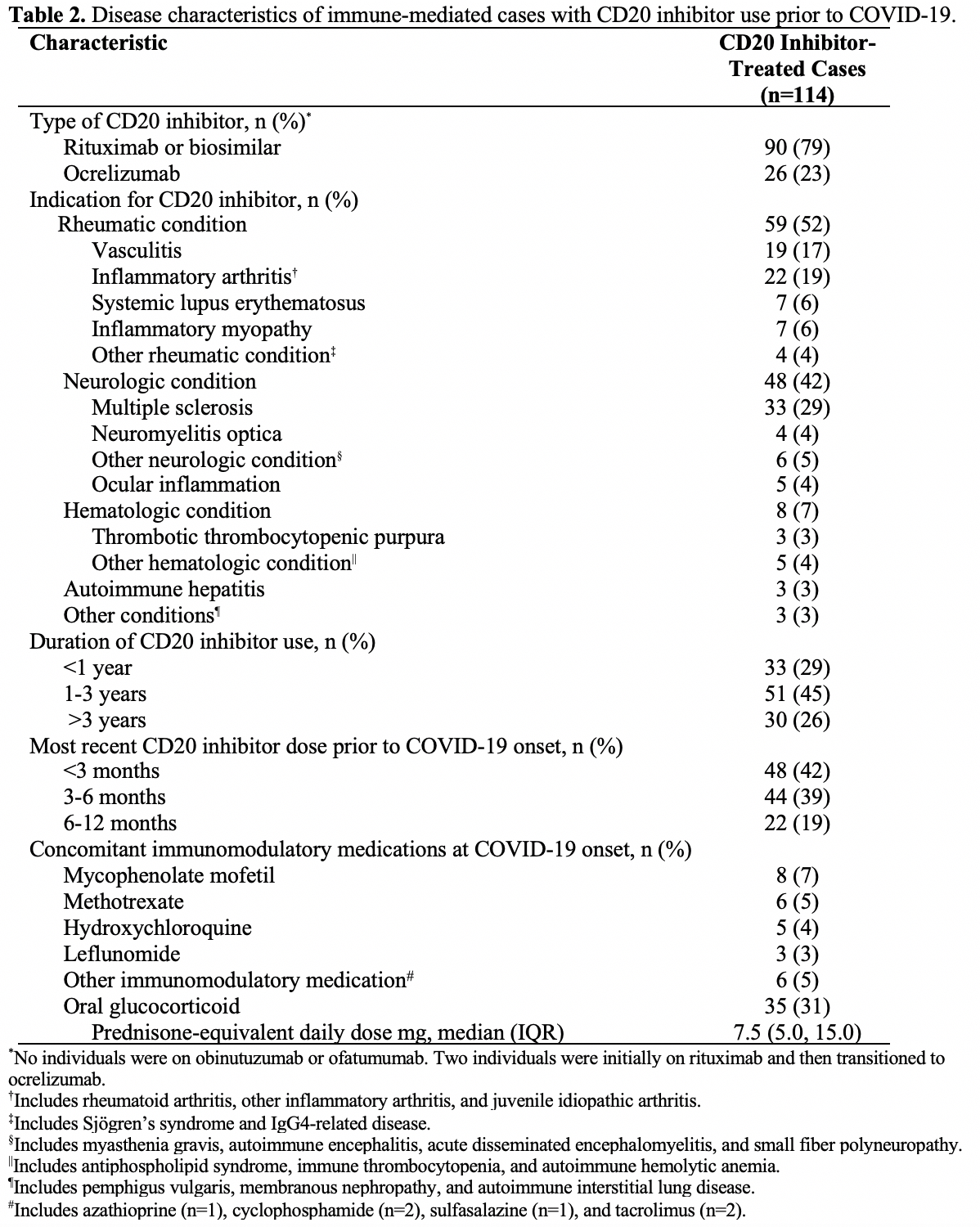
Results: We identified 114 cases with COVID-19 who used CD20 inhibitors for immune-mediated diseases and 559 matched comparators with COVID-19 (Table 1). Rheumatic disease (59 [52%]) and neurologic conditions (48 [42%]) were the most common indications for CD20 inhibition (Table 2). The total duration of CD20 inhibitor use was < 1 year in 33 (29%), 1-3 years in 51 (45%), and >3 years in 30 (26%). Forty-eight (42%) patients received a CD20 inhibitor dose within 3 months before COVID-19 onset. CD20 inhibitor-treated cases had higher mortality (aHR 2.16; 95% CI: 1.03 to 4.54) than matched comparators. Risks of hospitalization (aHR 0.88; 95% CI: 0.62 to 1.26) and mechanical ventilation (aHR 0.82; 95% CI: 0.36 to 1.87) were similar (Table 3). Approximately half of deceased patients in each group were not mechanically ventilated due to “Do Not Intubate” status. Deaths were numerically higher in patients on CD20 inhibitors for rheumatic diseases (7 [13%] vs. 15 [5%]), unadjusted HR 2.52; 95% CI: 1.07 to 5.90), which was attenuated in the adjusted model (aHR 1.76, 95% CI: 0.50 to 6.15). Short-term CD20 inhibitor users (< 1 year) had higher risk of death (7 [9%] vs. 11 [3%], unadjusted HR 2.82, 95% CI: 1.34 to 5.96) than comparators, which was attenuated in the adjusted model (aHR 2.33, 95% CI: 0.92 to 5.91). Lastly, those with long-term CD20 inhibitor use had numerically higher risk of death (5 [15%] vs. 10 [6%]) than comparators, and a similar trend in unadjusted (HR 2.92, 95% CI: 0.95 to 8.99) and adjusted (aHR 2.41, 95% CI: 0.66 to 8.87) models.
Conclusion: Patients who used CD20 inhibitors for immune-mediated diseases prior to COVID-19 infection had higher mortality than matched comparators. These results highlight the urgent need to mitigate excess risks in CD20 inhibitor users during the ongoing COVID-19 pandemic. Additional studies are needed to better stratify these risks and guide decision-making.
To cite this abstract in AMA style:
Patel N, D'Silva K, Hsu T, Di Iorio M, Fu X, Cook C, Prisco L, Martin L, Vanni K, Zaccardelli A, Zhang Y, Sparks J, Wallace Z. Association of CD20 Inhibitor Use with Severe COVID-19 Outcomes [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/association-of-cd20-inhibitor-use-with-severe-covid-19-outcomes/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-of-cd20-inhibitor-use-with-severe-covid-19-outcomes/