Session Information
Date: Sunday, October 26, 2025
Title: (0671–0710) Systemic Sclerosis & Related Disorders – Clinical Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Vasoactive-vasodilating drugs (VVD) are the cornerstone of the treatment of pulmonary arterial hypertension (PAH), a form of precapillary pulmonary hypertension (pPH) that represents a severe complication of systemic sclerosis (SSc). VVD include the categories of endothelin receptor antagonists (ERAs), phosphodiesterase type 5 inhibitors (PDE5i) and prostanoids, which are commonly used in SSc to treat digital ulcers (DU) and Raynaud’s phenomenon. As additional protective effects remain unclear, we investigated the effectiveness of VVD on the primary prevention of pPH and, specifically, of PAH.
Methods: SSc patients from the European Scleroderma Trials and Research (EUSTAR) cohort who underwent right heart catheterization (RHC) were included; postcapillary PH cases (pulmonary wedge pressure – PWP >15 mmHg) were excluded. Multivariable logistic regression assessed the association between exposure to VVD and detection of pPH (mPAP >20 mmHg, PVR>2 WU and PWP≤15 mmHg) and of PAH (pPH, ILD extent < 20% and FVC >70%). Models 1 & 2 tested the exposure at the time of RHC ever and ongoing to VVD categories (ERAs, PDE5i and prostanoids), models 3 & 4 tested the same for specific VVD molecules.The primary outcome was the diagnosis of precapillary PH; PAH was analyzed as sensitivity analyses.All models were adjusted for known confounders, including DLCO, age, current DU and systolic PAP on echocardiography. Interaction terms between VVDs and current DU were also tested.
Results: Among 944 eligible patients, 498 (53%) were diagnosed with pPH, of whom 367 (74%) had PAH (Table 1). For VVD classes, a statistically significant association was detected for the interaction of ERAs and current DU with the detection of pPH, in both logistic regression models 1 and 2 (Figure 1a and 1b). However, this finally resulted in a non-significant association between ERAs exposure in patients with current DU and PH detection when calculating marginal effects estimates (ERAs ongoing: OR 0.435, 95% CI 0.193 – 1.064; ERAs ever: OR 0.636, 95% CI 0.349 – 1.158). Additionally, both models showed lack of effectiveness of ERAs in patients without current DU, as well as for PDE5i or prostanoids overall. When focusing on specific VVD molecules, exposure “ever” to bosentan showed a significant protective association with precapillary PH diagnosis, independently from the presence or absence of current DU (Figure 1c). Finally, we noted again a statistically significant interaction between ongoing bosentan and current DU, which turned into a statistically significant marginal effects estimate (OR 0.230, 95% CI 0.081 – 0.652) indicating protective effects of this medication towards the diagnosis of precapillary PH in patients with current DU (Figure 1d). The protective effects of bosentan were confirmed in all sensitivity analyses targeting PAH detection.
Conclusion: Our data show that bosentan is associated with less frequent diagnosis of PAH and precapillary PH, in particular when employed in patients with current DU at the time of RHC. Our results support further research to optimize the timing and patient selection for VVD therapy in SSc, aiming also at additional preventive effects at pulmonary level.
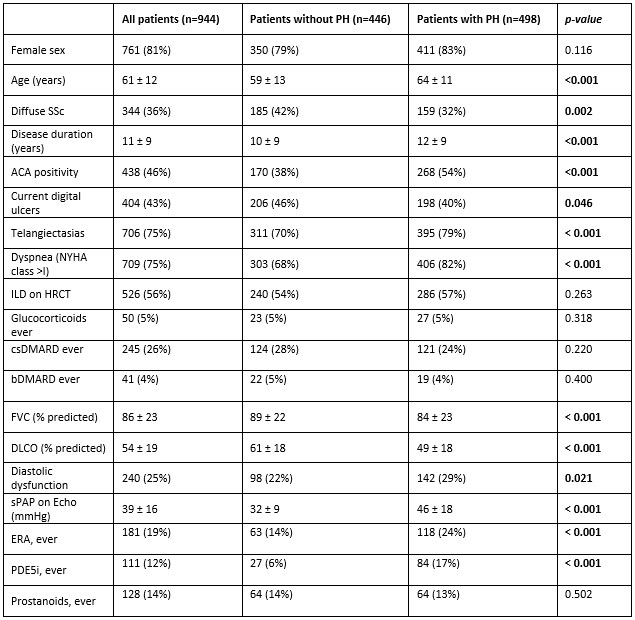 Table 1. Data about demographics, disease features, immunosuppressive and vasoactive treatment exposure and right heart catheterization from the study population, compared between patients with and without precapillary pulmonary hypertension.
Table 1. Data about demographics, disease features, immunosuppressive and vasoactive treatment exposure and right heart catheterization from the study population, compared between patients with and without precapillary pulmonary hypertension.
ACA, anti-centromere antibody; b/csDMARDs, biologic/conventional synthetic anti-rheumatic disease modifying drugs; DLCO, diffusion lung capacity of carbon monoxide; ERA, endothelin receptor antagonists; FVC, forced vital capacity; NYHA, New York Heart Association; PH, pulmonary hypertension; PDE5i, phosphodisterase 5 inhibitors; SSc, systemic sclerosis; sPAP, systolic pulmonary arterial pressure.
.jpg) Figure 1. Forest Plots of regression Models 1 (a), 2 (b), 3 (c), and 4 (d) evaluating the association between independent variables and the detection of precapillary pulmonary hypertension.
Figure 1. Forest Plots of regression Models 1 (a), 2 (b), 3 (c), and 4 (d) evaluating the association between independent variables and the detection of precapillary pulmonary hypertension.
ACA, anti-centromere antibody; DLCO, diffusion lung capacity of carbon monoxide; DU, digital ulcers; ERA, endothelin receptor antagonists; PAH, pulmonary arterial hypertension; sPAP, systolic pulmonary arterial pressure; PDE5i, phosphodisterase 5 inhibitors.
To cite this abstract in AMA style:
Farina N, Bellando-Randone S, SANGES S, Bjørkekjær h, tofani l, Truchetet M, Smith V, Balanescu A, Bergmann C, Allanore Y, Klemm P, Truglia s, Idolazzi L, Denton C, Foti R, Wojteczek a, Chatelus E, Vonk M, Guiducci S, Launay D, Hachulla E, de Vries-Bouwstra J, Hoffmann-Vold A, Matucci-Cerinic M, Distler O, Bruni C. Association Between Vasoactive-Vasodilating Therapy and Reduced Detection of Pulmonary Arterial Hypertension in Systemic Sclerosis: Evidence From a EUSTAR Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-between-vasoactive-vasodilating-therapy-and-reduced-detection-of-pulmonary-arterial-hypertension-in-systemic-sclerosis-evidence-from-a-eustar-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-vasoactive-vasodilating-therapy-and-reduced-detection-of-pulmonary-arterial-hypertension-in-systemic-sclerosis-evidence-from-a-eustar-study/
