Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: There is a high prevalence of knee osteoarthritis (OA) in people with type 2 diabetes (T2D), and knee OA increases risk for diabetes complications and cardiovascular events. Potential mechanisms linking symptomatic knee OA to worse outcomes in T2D include the effects of OA-related pain and immobility on blood glucose control and cardiorespiratory fitness, and systemic inflammation. Our objective was to assess the association between symptomatic knee OA and attainment of target blood glucose levels in individuals with T2D.
Methods: In this cross-sectional study, we recruited individuals with T2D aged ≥45 years from diabetes clinics at three academic hospitals in Toronto, Canada. Participants completed standardized online questionnaires that assessed demographics, comorbidities, height and weight, and joint symptoms. From clinic records we abstracted participants’ most recent HbA1c (within 3 months of questionnaire completion). Knee OA was defined as fulfilling NICE criteria (activity-exacerbated knee pain, morning joint stiffness ≤ 30 minutes) without diagnosis of inflammatory rheumatic disease. We considered diabetes blood glucose control at target if HbA1c was ≤7.0%. We used multivariable logistic regression to assess the association between knee OA and being at blood glucose target, adjusting for age and gender. We then examined the effect of further adjusting for body mass index (BMI), a risk factor for and consequence of knee OA. In secondary analyses, to understand effects in individuals who reported at least a mild average level pain over the past week, we repeated modelling with exposure of interest knee OA with knee pain ≥20/100 on pain numeric rating scale (NRS) (yes/no).
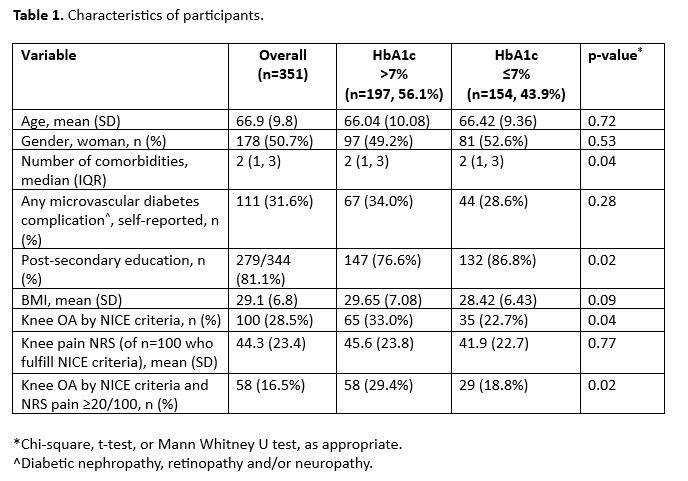
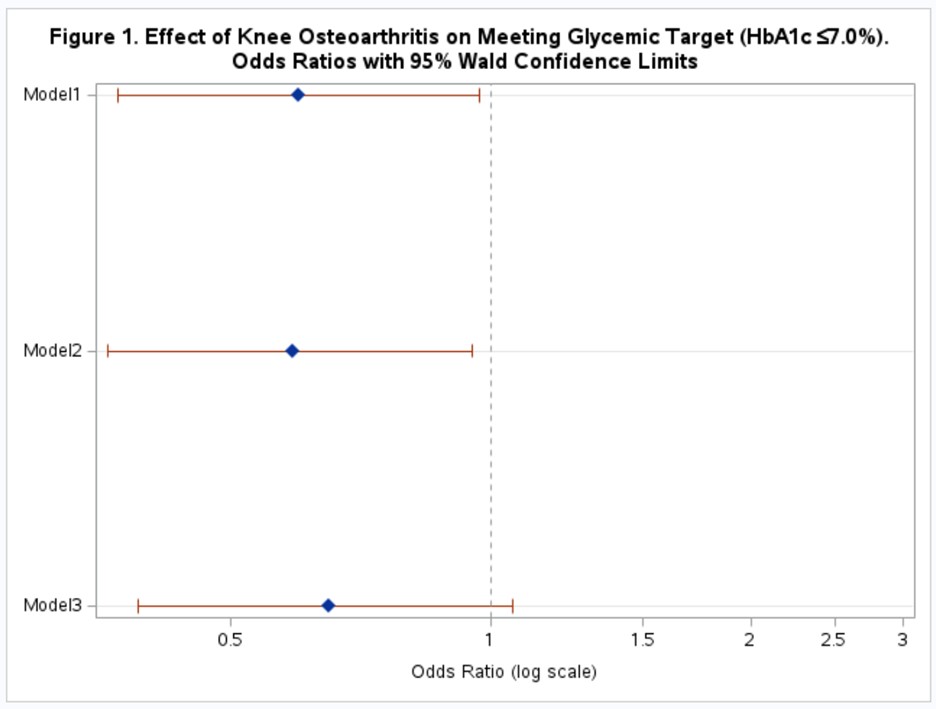
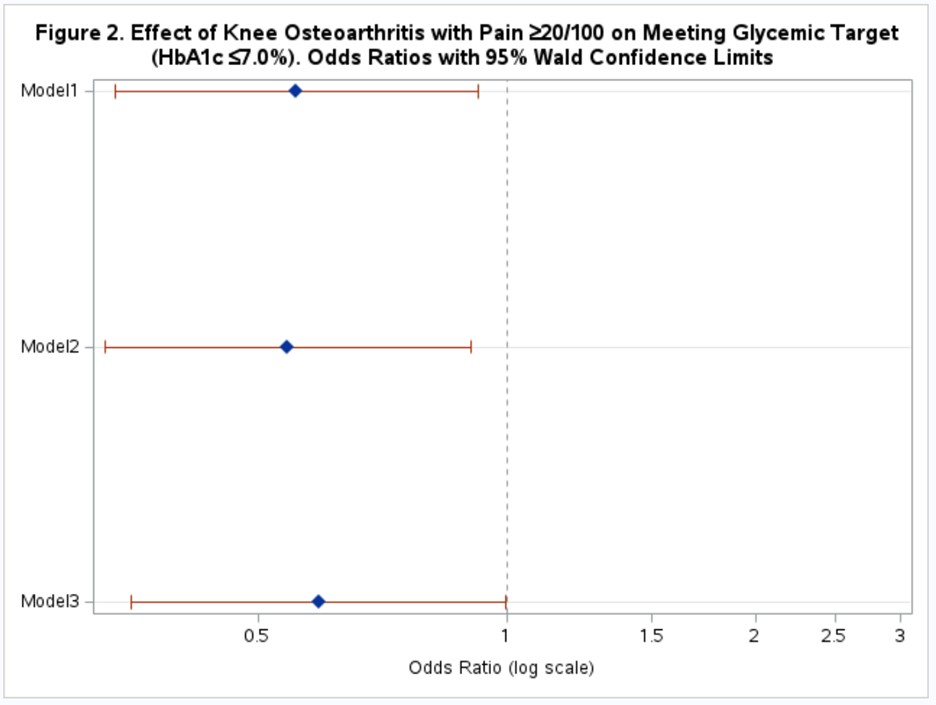
Results: We included 351 participants. Mean age was 66.9 (SD 9.8) years, 50.7% women, 81.1% had a post-secondary education, mean BMI 29.1 (SD 6.8) kg/m2, and 28.5% fulfilled NICE criteria for knee OA. Mean HbA1c was 7.4 (SD 1.2); 44% had HbA1c at target (≤7.0%) (Table 1). In univariable analysis, those with knee OA had lower odds of being at target (OR 0.60, 95% CI 0.37 to 0.97). Results were similar after adjusting for age and gender (OR 0.59, 95% CI 0.36 to 0.95). When further adjusting for BMI the effect of knee OA was attenuated and was not statistically significant (OR 0.65, 95% CI 0.39 to 1.06) (Figure 1). When exposure of interest was knee OA with self-reported pain ≥20/100, we found a stronger negative association; this met statistical significance even after adjusting for BMI (OR 0.59, 95% CI 0.35 to 0.997) (Figure 2).
Conclusion: Individuals with T2D with knee OA are less likely to be at the recommended target for glycemic control. This association was stronger for those who currently reported pain and remained significant even after adjusting for BMI. This suggests that symptomatic knee OA may increase risk of diabetes complications through worse glycemic control, and symptom severity is likely important. Future prospective studies with larger sample sizes are needed to better understand this relationship, as well as the role of additional mechanisms by which knee OA could lead to diabetes complications such as cardiorespiratory fitness and/or systemic inflammation.
Model 2: adjusted for age, gender
Model 3: adjusted for age, gender, BMI
Model 2: adjusted for age, gender
Model 3: adjusted for age, gender, BMI
To cite this abstract in AMA style:
King L, Weisman A, Shah B, Goldberg R, Parikh A, Stanaitis I, Nisenbaum R, Waugh E, Lipscombe L, Hawker G. Association Between Symptomatic Knee Osteoarthritis and Blood Glucose Control in Persons with Type 2 Diabetes [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-between-symptomatic-knee-osteoarthritis-and-blood-glucose-control-in-persons-with-type-2-diabetes/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-symptomatic-knee-osteoarthritis-and-blood-glucose-control-in-persons-with-type-2-diabetes/