Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Frailty is a state reflecting a reduced physiologic reserve. There is accumulating literature on the prevalence and clinical significance of frailty in Rheumatoid Arthritis (RA). A hospitalization with an in-hospital procedure represents a period of heightened stress posing a higher risk of adverse events. There is lack of evidence on the prevalence and prognostic significance of frailty in RA in the inpatient perioperative setting. We sought to assess the association between frailty and peri-procedure adverse outcomes.
Methods: We conducted a cross sectional study using data from the 2019 and 2020 National Inpatient Sample (NIS). Included were hospitalizations among ages ≥18 years who underwent a major diagnostic or therapeutic non-cardiac procedure and were discharged alive, and who underwent a major diagnostic or therapeutic non-cardiac procedure. Frailty was measured by the Hospital Frailty Risk Score (HFRS). RA status, procedures, comorbid diagnoses, and the HFRS were defined using International Classification of Diseases, Tenth Revision (ICD-10) codes. Procedures were categorized into low, intermediate, or high-risk using published guidelines. Outcomes of interest were all-cause inpatient mortality, adverse clinical events (ACE), and a need for higher discharge healthcare resources. ACE included the presence of myocardial infarction, acute congestive heart failure, major cardiac arrhythmia, deep venous thrombosis or pulmonary embolism, acute kidney injury, or wound infections. The discharge healthcare needs (DHN) was defined as need for skilled facility, home health. Logistics regression provided the Odds Ratio (OR) (RA vs. non RA) in both unadjusted [uOR] and adjusted for HFRS [aOR] models.
Results: Of the 9,979,407 hospitalizations, 1.9% had RA. RA patients were older (65.5 vs 54.4) and more likely to be women (74.7% vs 65.1%). Overall, 22.9% (RA vs non RA: 2.7% vs 23.4%) underwent low, 69.6% (RA vs non RA: 89.7% vs 68.3%) intermediate, and 7.4% (RA vs non RA: 7.7% vs 7.4%) high risk procedures.
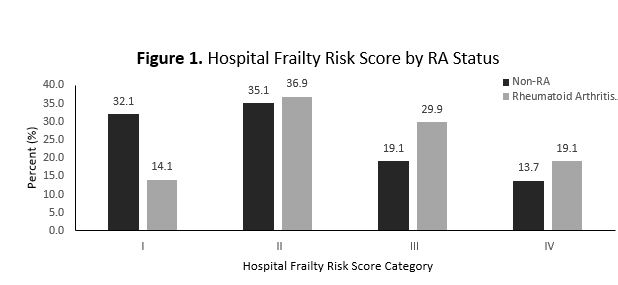
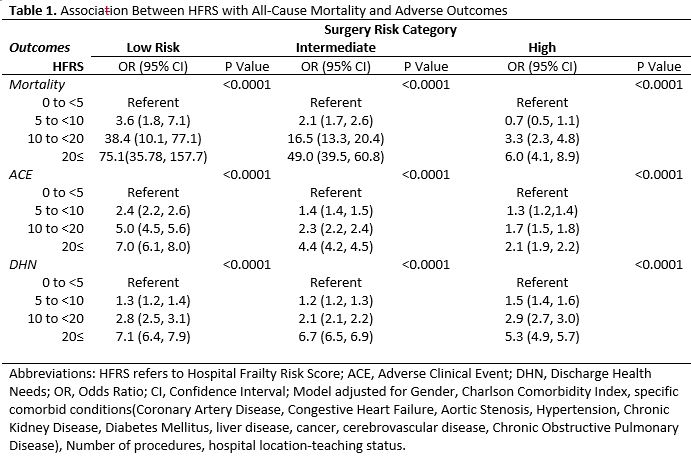
Patients were more likely to have higher HFRS (Figure 1). Table 1 displays the strong association between HFRS category and specific adverse events. For example, the uOR of all-cause mortality risk was 5.30 (95% Confidence Interval [CI]: 2.20 to 12.78) with aOR 0.91 (95% CI: 0.37 to 2.21), 0.70 (95% CI: 0.62 to 0.78) with aOR 0.59 (95% CI: 0.53 to 0.66), 0.75 (95% CI: 0.55 to 1.03) with aOR 0.73 (95% CI: 0.53 to 1.00) for low, intermediate, and high risk procedures, respectively. The uOR of ACE was 6.72 (95% CI: 5.86 to 7.71) with aOR 1.75 (95% CI: 1.39 to 2.22), 1.01 (95% CI: 0.97 to 1.04) with aOR 0.88 (95% CI: 0.84 to 0.91), 1.05 (95% CI: 0.95 to 1.16) with aOR 1.02 (95% CI: 0.92 to 1.13) for low, intermediate, and high risk procedures, respectively. The uOR of DHN was 6.64 (95% CI: 5.72 to 7.62) with aOR 2.38 (95% CI: 1.97 to 2.87), 1.75 (95% CI: 1.71 to 1.80) with aOR 1.65 (95% CI: 1.60 to 1.69), 1.16 (95% CI: 1.07 to 1.25) with aOR 1.11 (95% CI: 1.02 to 1.20) for low, intermediate, and high-risk procedures, respectively.
Conclusion: Frailty, as measured by HFRS, is prevalent in RA and strongly associated with adverse outcome. The use of this tool may serve an important role in preoperative assessment.
To cite this abstract in AMA style:
Yazdanyar A, Baker J, Wysham K, Ward M. Association Between Frailty and Peri-Operative Inpatient Adverse Outcomes Among Patients with and Without Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-between-frailty-and-peri-operative-inpatient-adverse-outcomes-among-patients-with-and-without-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-frailty-and-peri-operative-inpatient-adverse-outcomes-among-patients-with-and-without-rheumatoid-arthritis/