Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid Arthritis (RA) is associated with an increased risk of cancer, but the underlying risk factors remain poorly understood. Frailty is linked to an increased cancer risk in the general population and is more common among those with RA than those without it. We aimed to evaluate frailty as a risk factor for cancer in RA.
Methods: We used the Merative MarketScan databases from 2008 to 2022 to identify individuals with newly diagnosed RA using diagnosis codes and pharmacy records. Patients were then categorized as frail or non-frail based on Claims-based frailty index [1]. Incident cancer was identified using a validated algorithm in administrative claims data [2]. Following Cox proportional hazards models were created to obtain hazard ratios (HRs) and 95% confidence intervals (95% CIs) to evaluate the relationship between frailty and incident cancer: 1) unadjusted; 2) adjusted for demographics + Charlson comorbidity index (CCI); 3) adjusted for demographics + healthcare utilization and 4) adjusted for demographics + CCI + healthcare utilization.
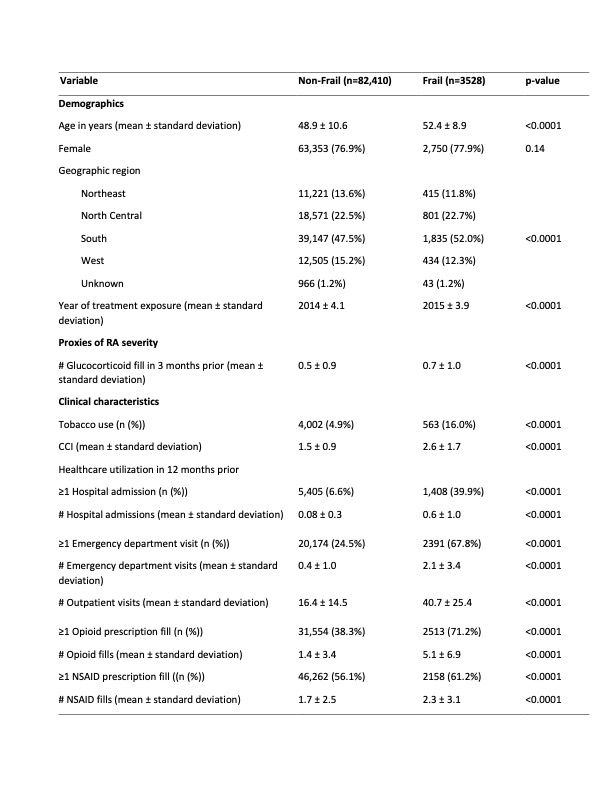
Results: We identified 85,938 individuals with new onset RA of whom 4.1% were frail. Frail patients were older than non-frail patients (52.4 ± 8.9 years vs. 48.9 ± 10.6 years), with higher tobacco use (16.0% vs. 4.9%) and mean higher Charlson comorbidity scores (2.6 ±1.7 vs. 1.5 ± 0.9). Additionally, frail patients had significantly higher healthcare utilization in the 12 months prior, with more hospital admissions, emergency department visits, outpatient visits, and medication fills compared to non-frail patients (Table 1).
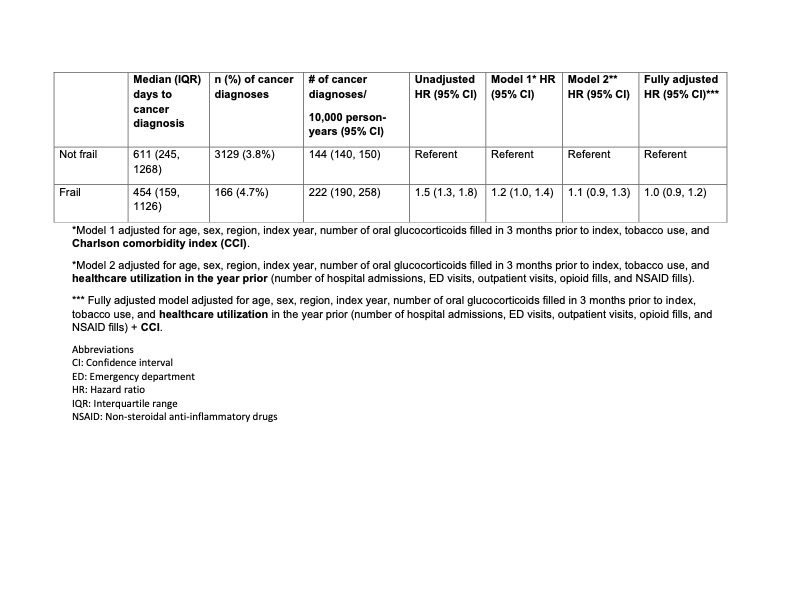
The median days to cancer diagnosis were shorter (454 days [interquartile range (IQR) 159, 1126] vs. 611 days [IQR 245, 1268]) and the incidence (95% CI) of cancer was higher (222 (190, 258) diagnoses per 10,000 person-years vs. 144 (140, 150) per 10,000 person-years) for frail patients compared to non-frail patients. After adjusting for demographics and CCI, the partial adjusted HR was 1.2 (95% CI: 1.0, 1.4). When additionally adjusted for healthcare utilization in the prior year, the fully adjusted HR was 1.0 (95% CI: 0.9, 1.2), indicating that frailty was not an independent predictor of cancer risk after controlling for these factors (Table 2).
Conclusion: Frail patients with newly diagnosed RA had higher baseline comorbidity and healthcare utilization, a higher unadjusted incidence of cancer, and shorter time to cancer diagnosis compared to non-frail patients. An association between frailty and incident cancer in RA cannot be ruled out given the small number of cancers in the frail group in this study.
References:
[1] Kim DH, Schneeweiss S, Glynn RJ, Lipsitz LA, Rockwood K, Avorn J. Measuring Frailty in Medicare Data: Development and Validation of a Claims-Based Frailty Index. J Gerontol A Biol Sci Med Sci 2018;73(7):980-987.
[2] Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. American journal of epidemiology 2011;173(6):676-682.
To cite this abstract in AMA style:
Bansal B, Gold L, Wysham K, Andrews J, Meara A, Presley C, Sharon E, Lee J, Barton J, Makris U, Singh N. Association Between Frailty and Incident Cancer in Newly Diagnosed Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/association-between-frailty-and-incident-cancer-in-newly-diagnosed-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-frailty-and-incident-cancer-in-newly-diagnosed-rheumatoid-arthritis/