Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: We investigated the association of frailty and delirium, both independently and in combination, with in-hospital mortality and non-routine discharge (i.e. when a patient is discharged to a destination other than their home, such as transfers to rehabilitation centers, or nursing homes) among hospitalized older adults with rheumatic diseases.
Methods: We performed a retrospective study using data from the Nationwide Inpatient Sample (NIS), spanning 2016 to 2022. Adults aged 65 and older with a primary diagnosis of select rheumatic diseases (rheumatoid arthritis. systemic lupus, polymyalgia rheumatica, psoriatic arthritis, giant cell arteritis, spondyloarthropathy) were identified using ICD-10 codes. Frailty and delirium were ascertained using the Hospital Frailty Risk Score (HFRS) (categorized into three levels: low (< 5), moderate (5–15), and high ( >15) frailty risk) and ICD-10 diagnostic codes, respectively. Multivariable logistic regression was used to assess the association of delirium and frailty both individually and combined with co-primary outcomes: in-hospital mortality and non-routine discharge. Each model was adjusted for demographic characteristics (age, sex, race and insurance status) and comorbidities. In a subgroup analysis, we evaluated these associations among patients with RA.
Results: Among 938,595 weighted hospitalizations of older adults with rheumatic diseases, 2.6% were classified as highly frail and 3.5% experienced delirium (Table 1). The mean age was 76.0 years, and 74.6% were female. Patients with RA comprised 70% of the cohort (Table 2). Both delirium and high frailty independently increased the odds of in-hospital mortality: delirium was associated with an OR of 4.99 (95% CI: 4.16–5.99) and high frailty with an OR of 6.80 (95% CI: 5.45–8.48). The combined presence of delirium and high frailty conferred the highest risk of mortality (OR: 16.2, 95% CI: 11.5–22.9). A similar pattern was observed for non-routine discharge, with elevated odds for delirium alone (OR: 3.14, 95% CI: 2.95–3.35), high frailty alone (OR: 5.69, 95% CI: 5.26–6.16), and both together (OR: 11.1, 95% CI: 8.78–14.0) (Figure 1). These associations remained significant across subgroup analyses.
Conclusion: Among hospitalized older adults with rheumatic diseases, both frailty and delirium were independently linked to poorer outcomes, including higher in-hospital mortality and increased likelihood of discharge to a non-home setting. Notably, patients with both conditions faced the greatest risk. These findings underscore the potential value of proactively identifying frailty and delirium during hospitalization, as doing so could help clinicians better support safe transitions out of the hospital.
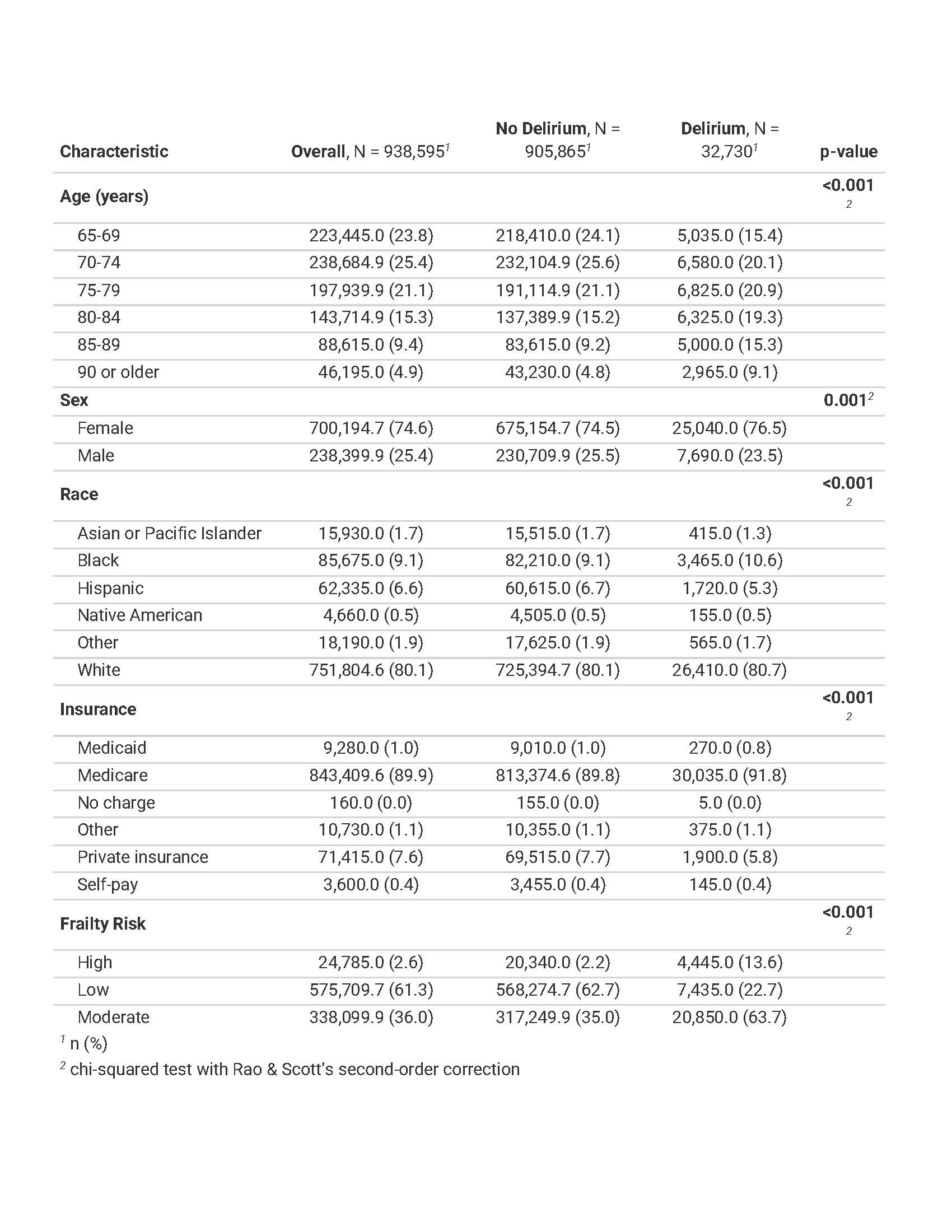 Table 1. Baseline characteristics of the cohort by delirium status.
Table 1. Baseline characteristics of the cohort by delirium status.
.jpg) Table 2. Breakdown of the cohort by rheumatic disease and delirium status.
Table 2. Breakdown of the cohort by rheumatic disease and delirium status.
.jpg) Figure 1. Multivariable analyses evaluating the association between frailty and delirium on a) in-hospital mortality and b) non-routine discharge among hospitalized older adults with rheumatic diseases.
Figure 1. Multivariable analyses evaluating the association between frailty and delirium on a) in-hospital mortality and b) non-routine discharge among hospitalized older adults with rheumatic diseases.
To cite this abstract in AMA style:
Bansal B, Jung Y, Damluji A, Goyal P, Singh N. Association between frailty and delirium and hospitalization outcomes among older adults with rheumatic diseases [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-between-frailty-and-delirium-and-hospitalization-outcomes-among-older-adults-with-rheumatic-diseases/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-frailty-and-delirium-and-hospitalization-outcomes-among-older-adults-with-rheumatic-diseases/
