Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Among adults, higher BMI contributes to worse outcomes and reduced response to treatment in rheumatoid arthritis (RA), but this relationship is understudied among those with Juvenile Idiopathic Arthritis (JIA). We investigated the relationship between BMI and disease activity 1-year post-diagnosis in JIA. Given that TNF inhibitors are the most commonly prescribed biologic DMARDs in JIA, we further assessed the impact of BMI category on response to treatment among those who were prescribed TNF inhibitors.
Methods: This is a retrospective cohort study from a single large quaternary center. Inclusion criteria were JIA (ages 2-16 years) diagnosed between November 2008 and September 2020 and followed for at least 12 months. Patients were identified using ICD-10 codes for JIA. Exclusion criteria were treatment with immunosuppressants before JIA diagnosis, inflammatory bowel disease, or missing data for height, weight, or disease activity at 12 months. Demographic characteristics, including height, weight, and BMI at initial rheumatology visit were extracted from a central patient database and patient clinic records. Age- and gender-specific BMI percentile was calculated for each patient and categorized according to CDC definitions as: underweight (< 5th percentile), healthy weight ( 5th to < 85th percentile), overweight (85th to < 95th percentile), or obese (≥ 95th percentile). Disease activity status at 12 months was extracted from patient records. Logistic regression was used to evaluate the association between BMI category and disease status overall and among those who were prescribed a TNF inhibitor (infliximab, etanercept, and adalimumab).
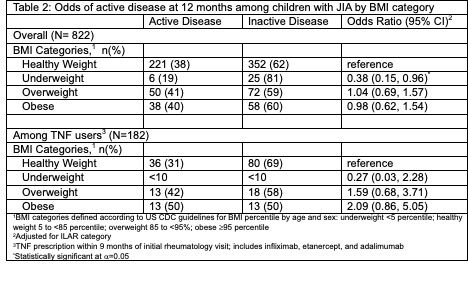
Results: Among 822 included patients, the majority (70%) were healthy weight (underweight: 4%, overweight: 15%, obese: 12%). Among 182 patients using TNF inhibitors, 64% were healthy weight (underweight: 5%, overweight: 17%, obese: 14%). Those who were underweight had lower odds of active disease at 12 months when compared to those with healthy weight, both overall (OR=0.38, 95%CI: 0.15-0.96) and among those taking TNF inhibitors (OR=0.30, 95%CI: 0.03-2.28). Among those taking TNF inhibitors, those who were overweight (OR=1.59, 95%CI: 0.68-3.71) or obese (OR=2.09, 95%CI: 0.86-5.05) had higher odds of active disease at 12 months compared to those with healthy weight.
Conclusion: Although it has been established in adults with RA that higher BMI contributes to worse disease outcomes, our analysis suggests that this may not be the case among children with JIA, as those who were overweight or obese had similar odds of active disease to those with healthy weight. Our study was likely underpowered to detect significant differences among those taking TNF inhibitors, but results suggest a trend, with higher likelihood of active disease found in each successively higher category of BMI. Further research in a larger cohort of JIA patients taking TNF inhibitors would elucidate the validity of this observed trend.
To cite this abstract in AMA style:
Sutton A, Shenoi S. Association Between Body Mass Index (BMI) and JIA Inactive Disease at One Year [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/association-between-body-mass-index-bmi-and-jia-inactive-disease-at-one-year/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/association-between-body-mass-index-bmi-and-jia-inactive-disease-at-one-year/

.jpg)