Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: While generally believed to be a safe, well-established treatment, hydroxychloroquine (HCQ) use is associated with irreversible retinal toxicity requiring regular monitoring. The objective of the study was to assess the association between HCQ and retinopathy in a rheumatology cohort and by indication utilizing a large longitudinal database.
Methods: Between January 1, 2011, to December 31, 2019, all rheumatology patients 18 years of age and older were identified within the DoD healthcare system. Patients were assigned exposure status by defining hydroxychloroquine (HCQ) utilization accessing pharmacy dispensing data using an intent-to-treat approach. Prior toxic retinopathy was an exclusion criteria. Propensity score (PS) matching (1:1) was used to create study cohorts balanced on baseline covariates, including indication in the overall cohorts. In the indication specific analyses, PS estimation and matching were performed in cohorts stratified by indication. Cox proportional regression modeling was used to estimate the hazard ratios of toxic retinopathy after exposure to HCQ among overall rheumatology cohorts as well as for rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE). All analyses were stratified by sex. A systematic algorithm was used to assign rheumatologic HCQ indication based on ICD-9/10 diagnostic codes assessed in claims data. Patients with diagnostic codes for a single rheumatologic condition were assigned that indication. If a patient had diagnostic codes for more than one rheumatologic condition, the indication with the most diagnostic codes was the defined indication. If one of the conditions was Sjögren’s, then the condition other than Sjögren’s, e.g., RA, was the assigned indication regardless of the count of diagnostic codes. SLE took precedence as the indication when diagnostic codes for both SLE and discoid lupus were present.
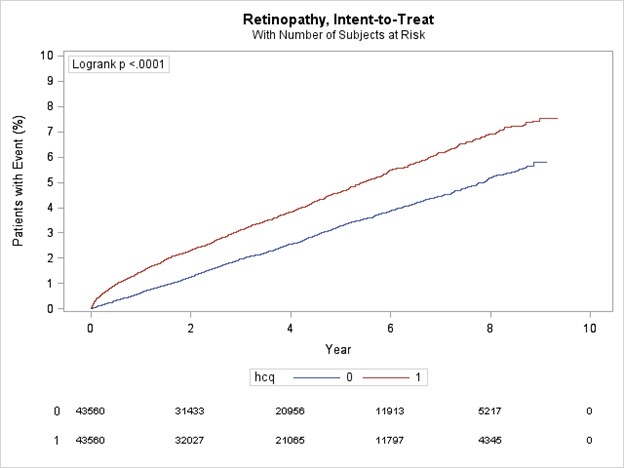
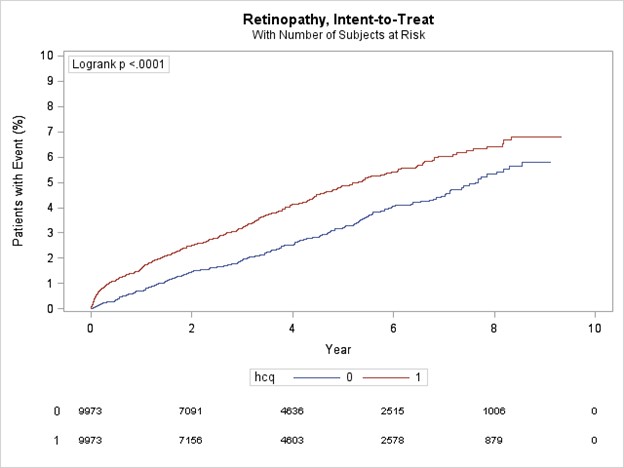
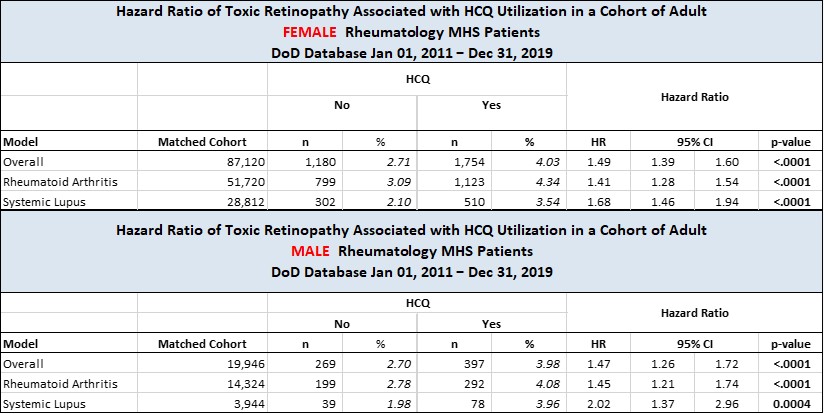
Results: All HCQ patients were matched to non-HCQ users. In the overall female cohort (n=88,120), patients had a mean age 55.7 (sd 16.6) and a median follow-up time 3.9 yr (IQR 1.9-6.2) and patients in the male cohort (n=19,946) had a mean age 60.8 (sd 16.0) and a median follow-up time 3.7 yr (IQR 1.8-6.1). In both cohorts, HCQ use was significantly associated (p< .0001) with retinopathy (Figure 1 & 2) with events occurring consistently more frequently in the HCQ cohorts. Female and male patients exposed to HCQ had a higher risk of retinopathy compared to non-exposed (HR 1.49, 95% 1.39,1.60; p< .0001; HR 1.47, 95% 1.26,1.72; p< .0001; respectively). For indications, HCQ use was significantly associated with retinopathy with variability seen within sex. The female RA cohort had an HR 1.41 (95% CI 1.28, 1.54; p< .0001) while the female SLE cohort had an HR 1.68 (95% CI 1.46, 1.94; p< .0001).A similar pattern was seen in the male cohorts, RA with HR 1.45 (95% CI 1.21, 1.74; p< .0001) and SLE with HR 2.02( 95% CI 1.37, 2.96;p=0.0004) (Table 1).
Conclusion: This uniquely large cohort of HCQ users reveals a risk of retinopathy that varies by sex and indication. The potential for serious ophthalmologic toxicity over the period studied emphasizes the importance of close ophthalmologic monitoring in the context of rheumatic disease where long term use is common.
To cite this abstract in AMA style:
Robbins R, Rush T, Edison J. Assessment of Association Between Hydroxychloroquine Use and Toxic Retinopathy, Overall and by Indication, in a Large Cohort of Rheumatology Patients Within the US Department of Defense Military Healthcare System [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/assessment-of-association-between-hydroxychloroquine-use-and-toxic-retinopathy-overall-and-by-indication-in-a-large-cohort-of-rheumatology-patients-within-the-us-department-of-defense-military-healt/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessment-of-association-between-hydroxychloroquine-use-and-toxic-retinopathy-overall-and-by-indication-in-a-large-cohort-of-rheumatology-patients-within-the-us-department-of-defense-military-healt/