Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The extent to which lack of adherence to prescribed treatment regimens contributes to differential disease outcomes in JIA – and demographic disparities in these outcomes – is unknown, largely because adherence is challenging to assess. Many methods rely on patient or caregiver report, which tend to overestimate adherence. Pharmacy dispensing data offer an objective means of assessing adherence through metrics such as the medication possession ratio (MPR), which measures the proportion of time a patient has medication available. We aimed to link medication adherence estimates to clinical data in the electronic health record (EHR) to investigate associations between medication adherence, disease activity, and patient characteristics.
Methods: This single-center retrospective cohort study leveraged pharmacy dispensing data from the EHR, provided by Surescripts, to calculate the MPR for MTX for patients with a physician diagnosis of JIA in a large pediatric rheumatology clinic. Surescripts is an information technology company that supports electronic prescriptions and provides this data to subscribing institutions.
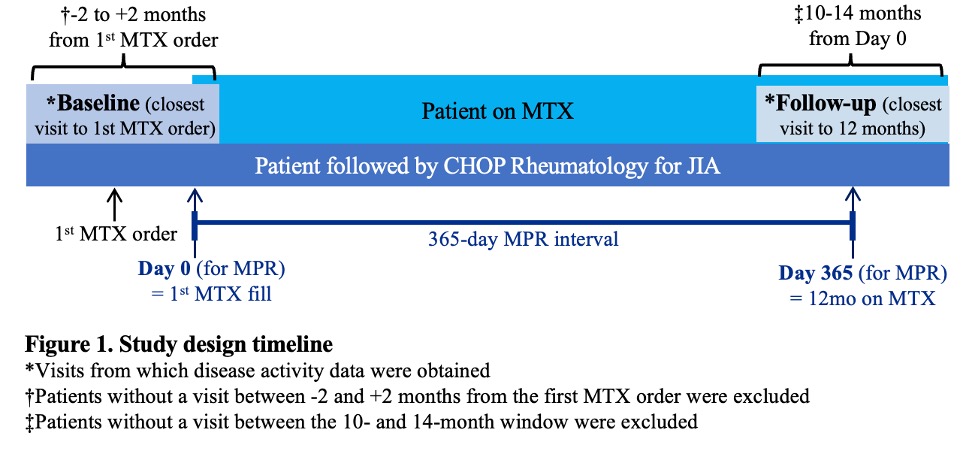
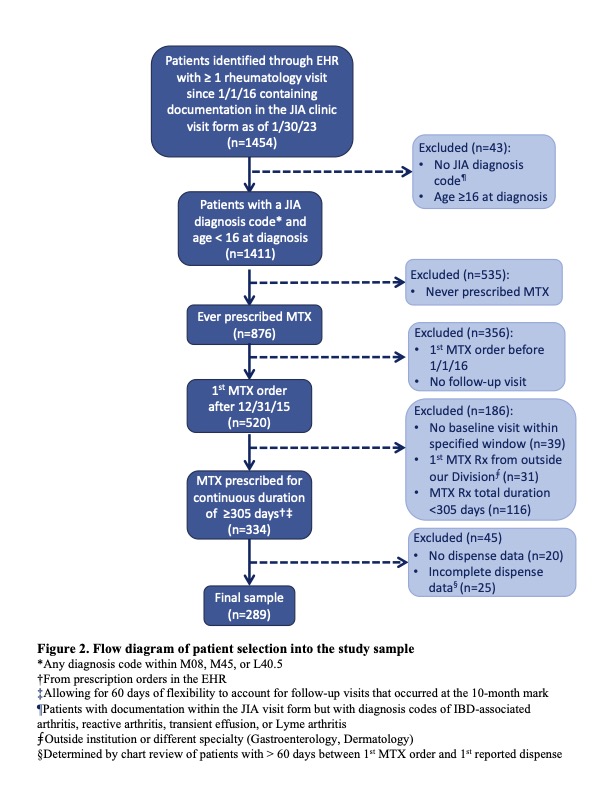
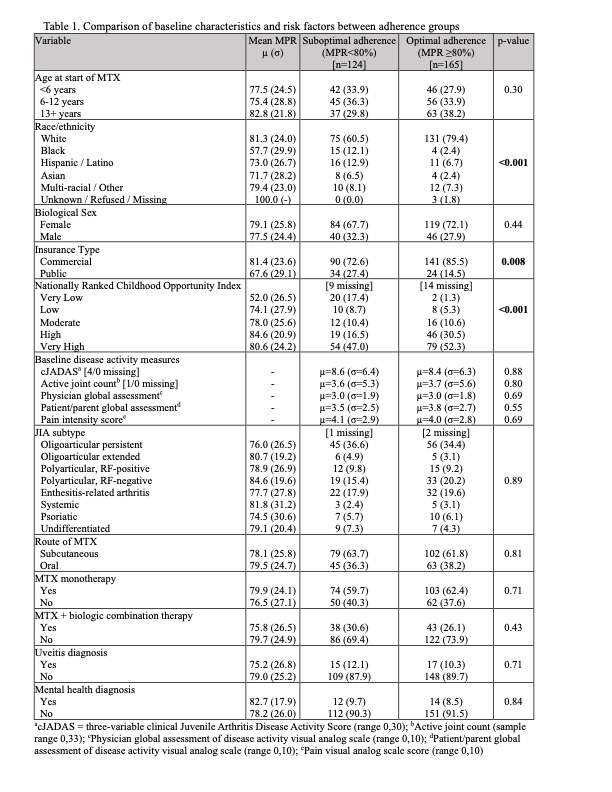
All incident users of MTX, treated between January 2016 and May 2022 for ≥12 months with outpatient rheumatology visits within 2 months of the first MTX prescription and after 12 months of follow-up (±2 months) (Figure 1), were included in the sample (Figure 2). MPR was calculated using the total days’ supply over a fixed 365-day interval following the initial MTX prescription fill date. Patient-level variables (Table 1), including sociodemographic factors and visit-level clinical factors from the baseline and follow-up visits, were extracted from the EHR. We dichotomized MPRs into optimal adherence (MPR ≥80%) and suboptimal adherence (MPR < 80%) groups. Patient characteristics were compared between the adherence groups using Fisher’s exact test for categorical variables and the Wilcoxon rank sum test for continuous variables.
Results: A total of 289 patients were included in the analysis (Figure 2). There was a mean of 9.4 dispenses per patient (SD 3.7) within the first year. Three patients had only 1 MTX dispense reported. The mean MPR was 84.5% (SD 32.3) and the majority (57.1%) of patients were classified as having optimal adherence. Patient race, public insurance, and a lower childhood opportunity index were associated with suboptimal adherence (Table 1). There were no statistically significant associations between adherence and disease activity at baseline, JIA subtype, route of MTX, concomitant use of biologics, or presence of uveitis or a mental health diagnosis.
Conclusion: Our findings demonstrate socioeconomic disparities in adherence to MTX among a cohort of patients with JIA. This method of linking dispense data to clinical data available in the EHR offers an objective approach to assessing adherence to chronic medications, but it should be validated against other methods. Future analyses will investigate associations between patient characteristics, MTX adherence, and disease activity using multivariable models. Qualitative work exploring patient perspectives on mechanisms that influence medication adherence will inform future adherence-focused interventions.
To cite this abstract in AMA style:
Abel D, Anderson D, Kallan M, Utidjian L, Chang J, Kenyon C, Gmuca S. Assessing Methotrexate Adherence in JIA Using Electronic Health Record-Linked Pharmacy Dispensing Data [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/assessing-methotrexate-adherence-in-jia-using-electronic-health-record-linked-pharmacy-dispensing-data/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessing-methotrexate-adherence-in-jia-using-electronic-health-record-linked-pharmacy-dispensing-data/