Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Rheumatoid arthritis (RA) associated autoantibodies, such as anti-citrullinated protein antibodies (ACPA), rheumatoid factor (RF) and anti-carbamylated protein antibodies (anti-CarP), can be present in serum years before clinical manifestation of RA. High ACPA-levels have been associated with a negative disease outcome. Recently, initiation of ACPA-response has been hypothesized to occur at inflamed mucosal surfaces, e.g., in the oral cavity. Therefore, it is of particular interest to investigate the IgA ACPA response and other IgA autoantibodies. The aim was to assess ACPA and anti-CarP autoantibodies levels (IgG and IgA) in serum of patients with mucosal inflammation at different sites, namely in periodontitis, cystic fibrosis and bronchiectasis patients, all without a diagnosis of RA.
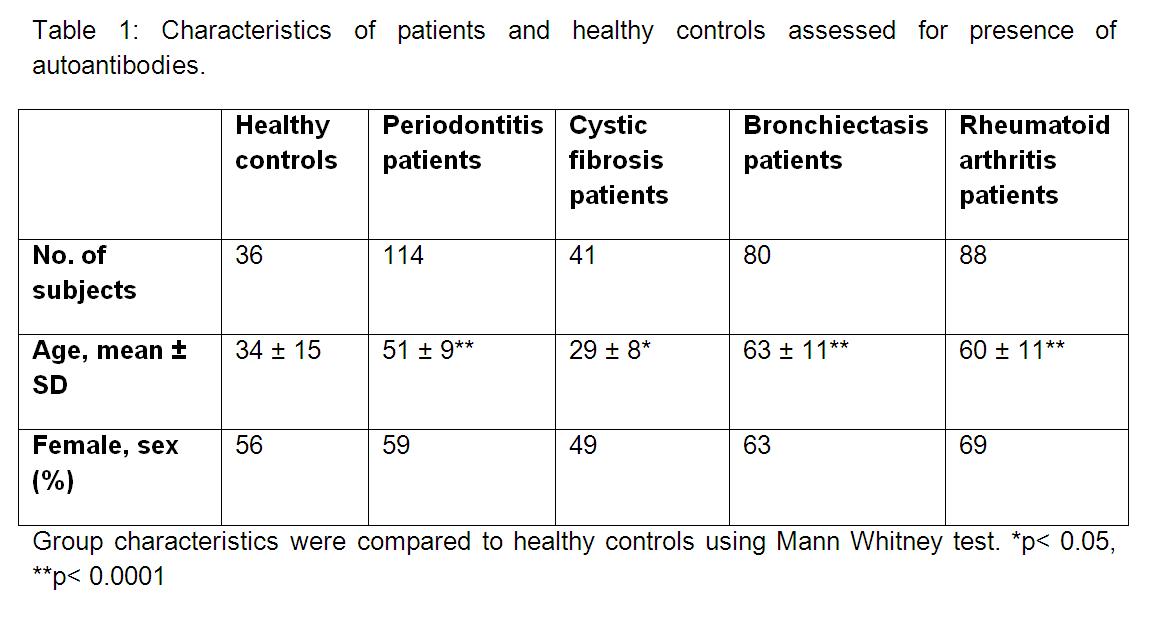
Methods: Autoantibody levels were assessed in periodontitis, cystic fibrosis and bronchiectasis patients. As controls, healthy subjects without periodontitis (HC) and a cohort of established RA-patients were added (Table 1). IgG anti-CCP2 levels were measured by ELISA (EuroDiagnostica, cut-off mean +2SD of HC). IgA anti-CCP2 levels were measured by a modified anti-CCP2 ELISA. Citrulline specificity of the anti-CCP2 response was assessed by measuring antibody levels against the arginine control peptide CAP (EuroDiagnostica). Serum IgM and IgA RF levels (cut-off >15, >25 IU/ml, respectively) and IgG antibodies against carbamylated FCS (cut-off mean +2SD of a distinct healthy control cohort) were measured by an in-house ELISA. IgG and IgA antibody levels against four citrullinated peptides (fibrinogen-1, 2, α-enolase and vimentin) were measured by ELISA in which the reactivity was corrected for the native peptides and positivity was defined as mean + 2SD of HC.
Results: Although RA autoantibody levels in periodontitis, cystic fibrosis and bronchiectasis patients were overall low, IgG seropositivity for anti-CAP (9.6%, 9.8% and 13.8%, respectively), anti-CCP2 (13.2%, 24.4% and 21.3%, respectively), and anti-CarP (3.5%, 7.3% and 3.8%, respectively) tended to be more prevalent in these groups compared to HC (5.6%, 5.6% and 0%, respectively). Comparable results were observed for IgA seropositivity. No increased seropositivity was observed for antibodies against the four citrullinated peptides. In bronchiectasis patients, seropositivity for IgM and IgA RF was significantly increased (18.8%, 23.8%) compared to HC (0%, 2.8%).
Conclusion: Presence of anti-CCP2 and anti-CarP is slightly more prevalent in serum of non-RA patients with mucosal inflammation. The increased levels of anti-CAP indicate that at least part of the increased anti-CCP2 reactivity might not be citrulline specific. In conclusion, our observations might be clinically relevant as we presume that once ACPAs are initiated they can mature in individuals that are genetically pre-disposed for RA.
Disclosure:
K. M. J. Janssen,
None;
M. J. de Smit,
None;
E. Brouwer,
None;
B. Doornbos-van der Meer,
None;
A. J. van Winkelhoff,
None;
A. Vissink,
None;
J. Altenburg,
None;
N. Levarht,
None;
M. K. Verheul,
None;
L. A. Trouw,
None;
J. Westra,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/arthritis-associated-autoantibodies-in-non-rheumatoid-arthritis-patients-with-mucosal-inflammation/