Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Non-steroidal anti-inflammatory drugs (NSAIDs) are the keystone in the treatment of axial Spondyloarthritis (axSpA), and even in early forms, patients symptoms may lead to an over-treatment by NSAIDs. However, the current recommendation is to use NSAIDs at the lowest efficacious dose for the shortest period of time, due to safety issues (cardiovascular and gastro-intestinal side effects). The aim of our study was to describe the real-life NSAID use in an observational cohort of inflammatory back pain suggestive of axial SpA over a 3 years period of follow-up.
Methods: Study design: Observational prospective, multi-centre study (DESIR cohort) of patients with early inflammatory back pain (IBP) suggestive of ax-SpA. Patients: Patients who attended all 6 visits (every 6 months during the fist 2 years and yearly at 3 years) and for whom NSAID information was available were included in this analysis. Data collected at every visit over 3 years: NSAID intake and ASAS-NSAID intake score for the 6 months preceding the visit. The ASAS-NSAID intake score reflects the overall intake of NSAID during a period and ranges from 0 to 200 or more (where a 100 =150 mg of Diclofenac/day every day of the period of interest); “highly doses” were defined as score > 75. Statistical analysis: descriptive analysis of the NSAID intake (as a binary variable “NSAID intake during the last 6 months” yes/no, and as a continuous variable by the ASAS-NSAID intake score for the last 6 months). Variation of the ASAS-NSAID score over time was tested by analysis of variance (ANOVA).
Results: 627 patients (46.1% males, mean age 33.7(8.7)) were assessed. 181 (28.9%) patients received a least one TNF alpha blocker during follow-up. At inclusion, 582 patients (92.8%) patients were taking NSAIDs; this proportion decreased over time, with the lowest proportion being 70.2% at 18 months. At all visits, more than 70% patients were treated with NSAIDs. Median ASAS-NSAID intake score was 36 (13-72) at inclusion, and substantially decreased to reach 7 (0-44) after 3 years (p<0.0001) (Figure) “Highly treated” patients represented 10% of the population at inclusion, and 4% after 3 years, with only 3 patients with a sustained score > 100 over time.
Conclusion: more than 70% of this early axSpA population received an NSAID treatment over the 3-years of follow-up, but intake significantly decreased over time, with only very few “highly treated” patients. This suggests that rheumatologists do not over-treat early axSpA patients with NSAIDS. Further studies should focus on those patients with sustained high doses of NAIDS over time.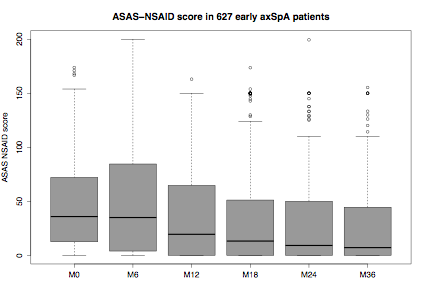
Disclosure:
A. Moltó,
None;
B. Granger,
None;
D. Wendling,
None;
M. Dougados,
None;
L. Gossec,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/are-we-over-treating-with-nsaids-our-early-axial-spa-patients-results-from-the-desir-cohort/
