Session Information
Date: Saturday, November 12, 2022
Title: Spondyloarthritis Including PsA – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Treatment success from the patients’ perspective has not been defined in psoriatic arthritis (PsA). The objective was to determine prevalence and associations of patient-reported treatment success in PsA.
Methods: Consecutive patients with rheumatologist-diagnosed PsA, meeting the CASPAR classification, were recruited from a single center. The intervention was PsA guideline-based standard of care, which is defined as a review of disease activity and medication safety every 3-6 months and adjustment of therapy to meet treatment targets of low disease activity or remission (1-3). PsA outcome measures collected included: 68/66 tender/swollen joint counts, Leeds/SPARCC enthesitis indices, Leeds dactylitis index, psoriasis body surface area, patient reported outcomes (patient global, pain, PROMIS-29 Profile and additional short forms) and the patient acceptable treatment state (PASS). Treatment targets using DAPSA and MDA were calculated. The study primary outcome was a single-item question that assessed the patient’s impression of treatment success: “Today, considering the level of control of your psoriatic arthritis and psoriasis, do you consider your treatment has been successful?” with response options Yes/No. A “No” choice branched to a drop-down list of reasons patients could select. Treatment success groups were compared using Student-t, Wilcoxon and Fisher’s exact tests.
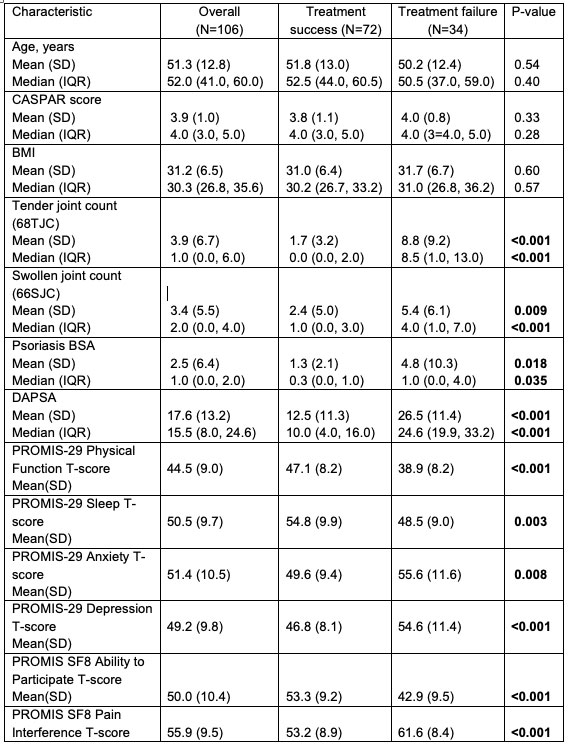
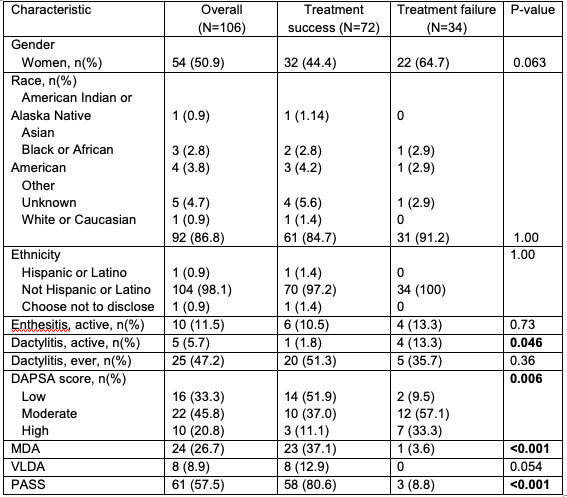
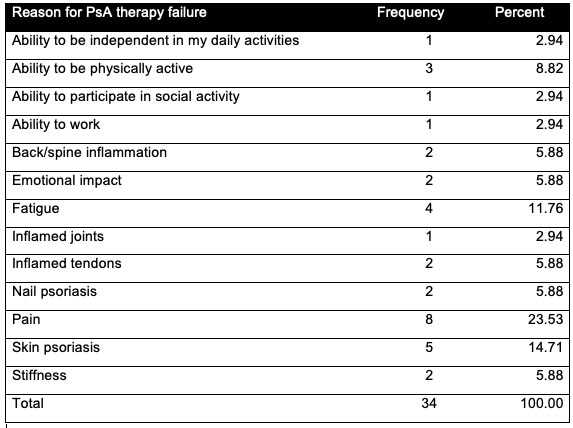
Results: A total of 106 participants had a baseline visit. Mean(SD) CASPAR score was 3.9 (1.0), mean age 51(13) years, mean BMI 31(7), 51% women, and 87% Caucasian. Seventy-two (68%) reported treatment success, and versus not, had significantly lower tender/swollen joint counts, dactylitis, psoriasis, and were more likely at treatment target by DAPSA and MDA; they also had better quality of life according to PROMIS-29 domains (Table 1a and b). Demographics and BMI were not associated with patient-reported treatment success. The most common reasons patients chose for treatment failure were pain (24%), psoriasis (15%), fatigue (12%) and decreased ability to be physically active (9%) (Table 3).
Conclusion: Patient-reported treatment success in PsA was associated with control of arthritis, dactylitis, psoriasis, and health-related quality of life. The top three patient-reported reasons for treatment failure were pain, psoriasis and fatigue.
References 1. Singh JA, Guyatt G, Ogdie A, Gladman DD, Deal C, Deodhar A, et al. Special Article: 2018 American College of Rheumatology/National Psoriasis Foundation Guideline for the Treatment of Psoriatic Arthritis. Arthritis Rheumatol 2019;71:5–32.
2. Gossec L, Baraliakos X, Kerschbaumer A, Wit M de, McInnes I, Dougados M, et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2019 update. Ann Rheum Dis 2020;79:700–712.
3. Coates LC, FitzGerald O, Merola JF, Smolen J, Mens LJJ van, Bertheussen H, et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis/Outcome Measures in Rheumatology Consensus-Based Recommendations and Research Agenda for Use of Composite Measures and Treatment Targets in Psoriatic Arthritis. Arthritis Rheumatol 2018;70:345–355.
To cite this abstract in AMA style:
Samuel C, Prichett L, Grader-Beck T, Haque U, Miller J, Grieb S, Orbai A. Are We Meeting Patients’ Treatment Goals with Guideline-Based Therapy for Psoriatic Arthritis? [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/are-we-meeting-patients-treatment-goals-with-guideline-based-therapy-for-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/are-we-meeting-patients-treatment-goals-with-guideline-based-therapy-for-psoriatic-arthritis/