Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Neuropsychiatric (NP) symptoms occur in >50% of patients with systemic lupus erythematosus (SLE). A major barrier to research includes the non-specific nature of neuropsychiatric syndromes and the uncertainty of attribution to SLE activity. Unmet needs in NPSLE research include recognizing neuropsychiatric symptoms in lupus, diagnostic biomarkers, diagnostic imaging, prognostication, and novel therapies.
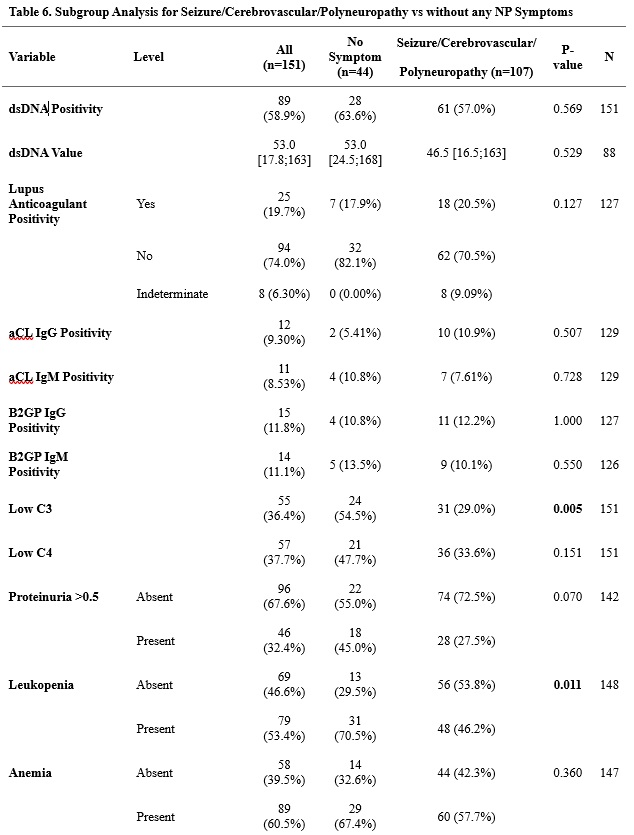
Methods: Charts of patients at a large academic center registry were reviewed to record the prevalence of the 19 NP symptoms described by the ACR in 1999. Patient demographics (gender, age, race, disease phenotype, disease duration), SLEDAI 2k score, autoantibody status, C3/C4 levels, and proteinuria >0.5 mg/mmol were collected from chart review. The number of hospitalizations, number and type of current and past immunosuppressive therapies as well as non-immunosuppressive therapies for patients with NP symptoms were compared to those without. Subgroup analysis was performed for those patients with seizure/cerebrovascular disease/polyneuropathy.
Results: 334 charts were reviewed, 327 were included in statistical analysis. 89% of patients were female, 11% male. By race, 65.9% White, 30.6% African American, 2.19% Asian, and 1.25% Hispanic/Latino. NP symptoms were present in 86.5% of the cohort, the most common were: headache (59.3%), anxiety (55.1%), mood disorder (49.8%), cognitive dysfunction (42.5%), polyneuropathy (20.3%), seizure (9.2%), and cerebrovascular disease (8%). There was no statistically significant difference in hospitalizations or immunosuppressive therapies utilized in patients with NP symptoms compared to those without. However, patients with NP symptoms were more often hospitalized between 2-10 times compared to those without NP symptoms (not statistically significant). Patients with NP symptoms were more often on current steroid therapy and less often on current azathioprine, mycophenolate, or anifrolumab, and less often received past azathioprine or mycophenolate therapy (not statistically significant). Patients with NP symptoms were statistically more likely to be on antiepileptics (p=0.002), antidepressants (p< 0.001), or benzodiazepines (p=0.007). In subgroup analysis, patients with seizure/cerebrovascular disease/polyneuropathy were less likely to have low C3 (p=0.005) or proteinuria >0.5 (p=0.070) but were more likely to have leukopenia (p=0.011), be hospitalized (p=0.318), receive IVIG (p=0.04), antiepileptics (p< 0.001), antipsychotics (p=0.034), antidepressants (p< 0.001), and benzodiazepines (p=0.003).
Conclusion: There was no statistical difference in hospitalizations or immunosuppression between patients with NP symptoms versus those without. However, patients with NP symptoms were more often hospitalized between 2-10 times compared to patients without NP symptoms and were more often on current steroid therapy, and statistically more often on an antiepileptic, antidepressant, or benzodiazepine therapy. Patients with seizure/cerebrovascular disease/polyneuropathy were statistically less likely to have low C3 (p=0.005) but were more likely to have leukopenia (p=0.011).
To cite this abstract in AMA style:
Vondenberg J, Zhang C, Littlejohn E. Are Neuropsychiatric Symptoms in Systemic Lupus Erythematosus (NPSLE) Associated with More Frequent Hospitalizations or Exposure to a Greater Number of Immunosuppressive Medications? [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/are-neuropsychiatric-symptoms-in-systemic-lupus-erythematosus-npsle-associated-with-more-frequent-hospitalizations-or-exposure-to-a-greater-number-of-immunosuppressive-medications/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/are-neuropsychiatric-symptoms-in-systemic-lupus-erythematosus-npsle-associated-with-more-frequent-hospitalizations-or-exposure-to-a-greater-number-of-immunosuppressive-medications/