Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid syndrome (APS) has been classified as the development of venous and/or arterial thromboses, and/or pregnancy morbidity, in the presence of persistently raised levels of the circulating antiphospholipid antibodies, namely lupus anticoagulant (LAC), anticardiolipin (aCL) and anti-β2-glycoprotein I. APS is a significant cause of morbidity and mortality in patients with Systemic Lupus Erythematosus (SLE). It is well known that LAC positivity is more strongly associated with both arterial and venous thrombosis than either aCL or anti-β2glycoprotein I antibodies in SLE. An unanswered question is the contribution of different combinations of positive antiphospholipid antibodies to thrombosis risk. We evaluated which antiphospholipid antibody combinations increased the risk of future thrombosis in patients with SLE.
Methods: This prospective analysis included SLE patients who had been tested for all 7 antiphospholipid antibodies: lupus anticoagulant (LAC), anticardiolipin (aCL) isotypes IgM, IgG, IgA, and anti-β2-glycoprotein I isotypes IgM, IgG, IgA. We excluded RVVT measures if patients were taking anticoagulants (warfarin/ heparin). We constructed a dataset with one record per month of follow up for each patient. Rates of thrombosis for each antiphospholipid or each combination of antiphospholipid antibody were calculated as the number of thromboses divided by the number of person-months at risk and the results are converted to rates per 1000 person-years. To assess the relationship between antiphospholipid antibodies and thrombosis, we used pooled logistic regression.
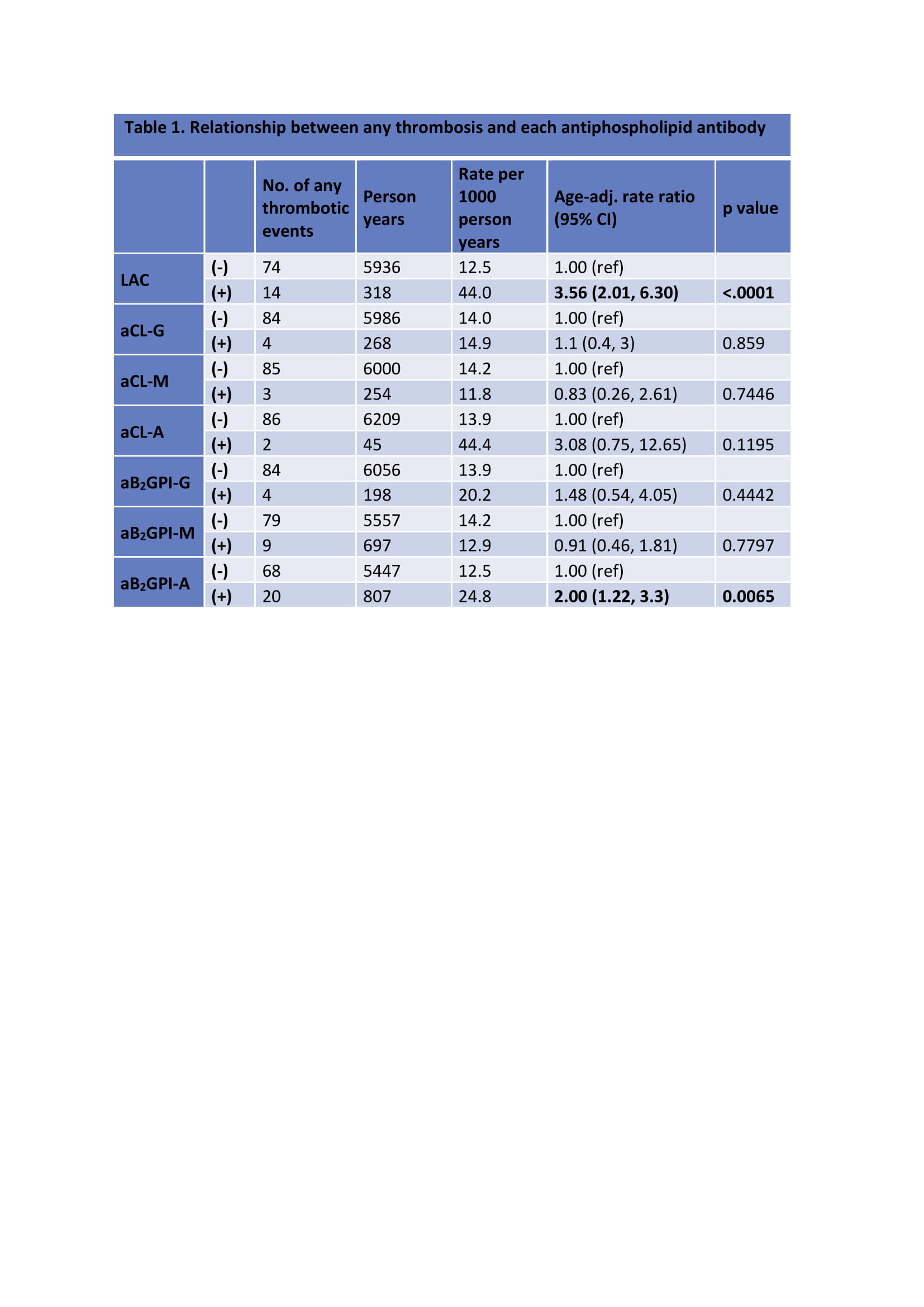
Results: There were 821 patients with a complete profile of 7 antiphospholipid antibodies with a total of 75048 person-months of follow up. Among these patients, there were 88 incident cases of thrombosis: 48 patients with arterial, 37 patients with venous and three patients both with arterial and venous thrombosis.In individual models; LAC was the most predictive of any [3.56 (2.01, 6.30) p< 0.0001], venous [4.89 (2.25, 10.64) p< 0.0001], and arterial [3.14 (1.41, 6.97) p= 0.005] thrombosis. Anti-β2-glycoprotein I IgA positivity was a significant risk factor for any [2.00 (1.22, 3.3) p=0.0065] and venous [2.8 (1.42, 5.51) p=0.0029] thrombosis. We looked at patients who were LAC positive and asked if having another positive antiphospholipid antibody increased the risk ratio for any, venous, and arterial thrombosis. We found that having anti-β2-glycoprotein I IgA appeared to add significant risk to any [1.73 (1.04, 2.88) p=0.0362], and venous [2.27 (1.13, 4.59) p=0.0218] thrombosis among those with or without LAC.
Conclusion: Our study shows that LAC is still the best predictor of risk of any, arterial and venous thrombosis in SLE. Moreover, anti-β2glycoprotein I IgA positivity appeared to add significant risk for any and venous thrombosis. The clinical significance of IgA anti-β2glycoprotein I deserves further investigation in SLE patients.
To cite this abstract in AMA style:
Demir S, Li J, Magder L, Petri M. Antiphospholipid Patterns Predict the Risk of Thrombosis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/antiphospholipid-patterns-predict-the-risk-of-thrombosis-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/antiphospholipid-patterns-predict-the-risk-of-thrombosis-in-systemic-lupus-erythematosus/