Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is characterized by positive antibodies to dsDNA and/or Sm which have high specificity for the disease. While anti-dsDNA titers are known to vary with lupus disease activity, this is not clear for anti-Sm. The objectives of this study were to investigate whether anti-Sm titers vary during SLE disease course and correlate with disease activity and response to treatment.
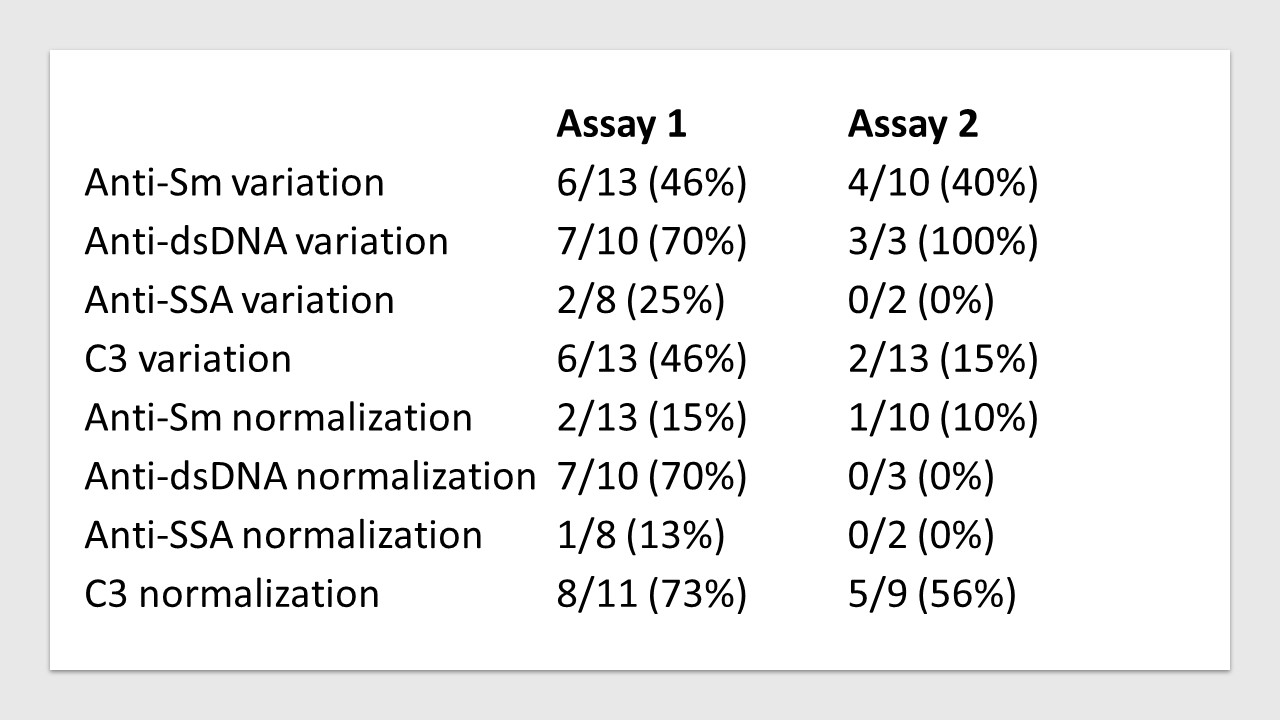
Methods: We identified a total of 37 SLE patients from the rheumatology practice of one of us (KK) at an academic center who had office visits between 2/1/2016 and 4/30/2023 and had at least 2 positive values of anti-Sm during follow up. They all met the 2019 SLE classification criteria. To date, we have studied 22 of those patients. We have collected demographic data, disease duration, and serologic data for anti-Sm, dsDNA, SSA titers, as well as C3 levels. We set the date of the first positive anti-Sm value for each patient as the baseline date for the start their follow-up which concluded at the last date with available anti-Sm data or the end of study. Antibody (Ab) variation was defined as present if a change in anti-Sm titers by more than 50% of the highest value occurred during follow-up, whereas Ab normalization if anti-Sm titers became negative. We looked for similar changes for anti-dsDNA, anti-SSA, and C3. We analyzed available serologic data obtained by our institution’s laboratory (Assay 1) and a commercial assay (Assay 2) separately.
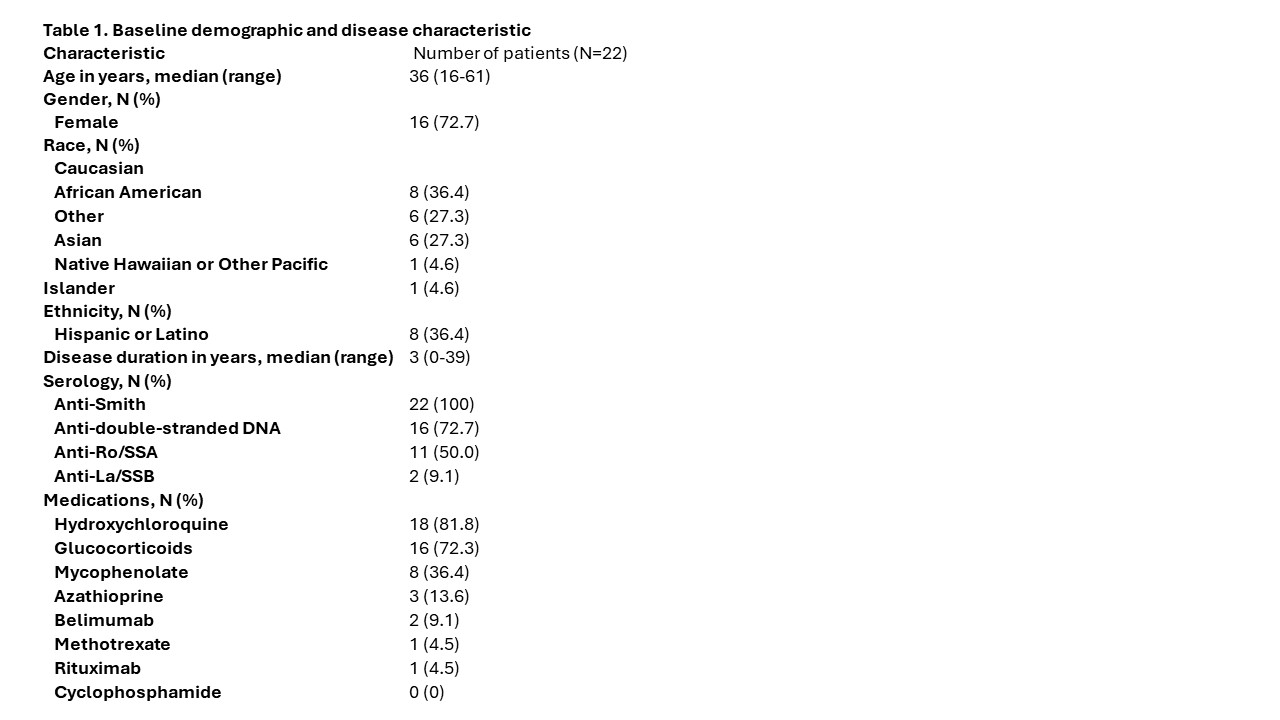
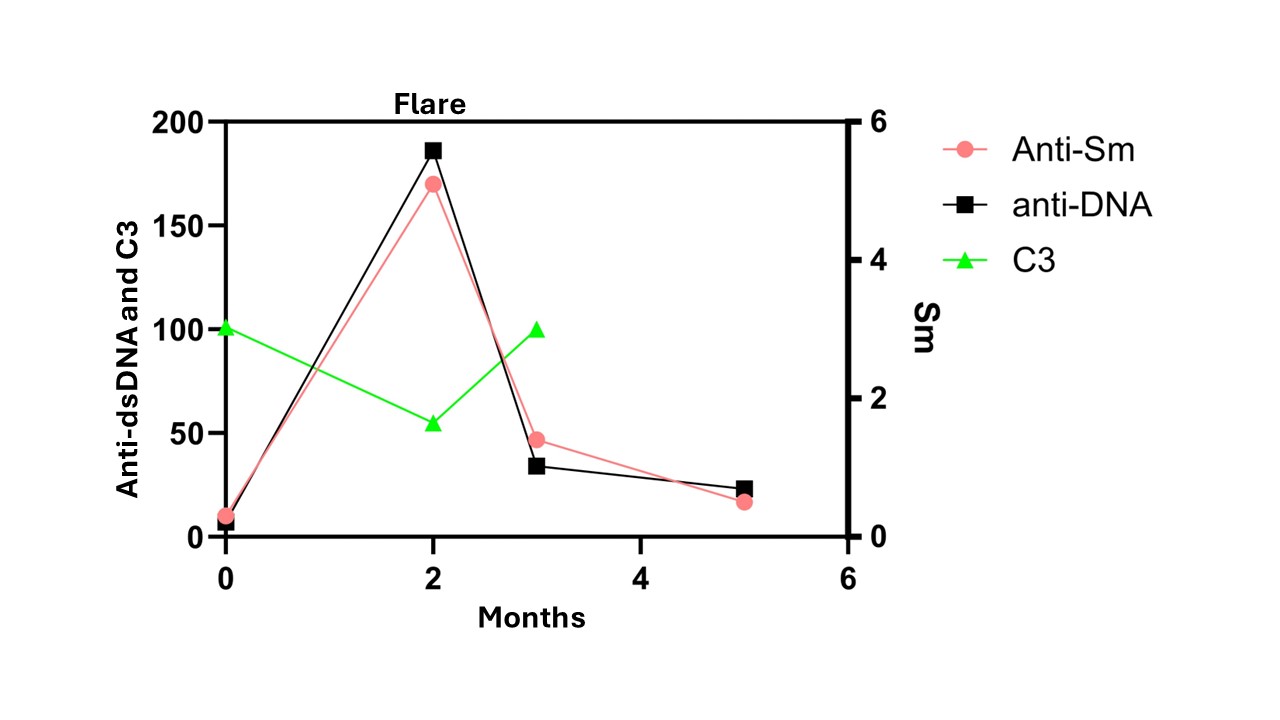
Results: Table 1 shows the demographic, and other data for the 22 patients studied. The majority of patients were non-Caucasians (Table 1). Anti-Sm Ab variation occurred in 6/13 patients (46%) and 4/10 (40%) by assay 1 and 2 respectively. In comparison, anti-dsDNA variation occurred in 70% and 100% whereas anti-SSA variation occurred only in 13% and 0% by the 2 assays respectively. Similarly, normalization rates appeared to occur in anti-Sm titers less frequently compared to those for anti-dsDNA and more frequently to those for anti-SSA. C3 normalization rates were as expected: 53-73%. Of note, one patient had anti-Sm and anti-dsDNA positive seroconversions during a severe lupus flare (pleurisy and nephritis) that was treated aggressively with pulse followed by high dose oral glucocorticoids and mycophenolate. Substantial downregulation of both Ab titers followed along with resolution of the flare in a few months.
Conclusion: Anti-Sm antibody titers may vary greatly during lupus disease course, although not to the same extent as anti-dsDNA titers, in contrast to anti-SSA titers that are less amenable to change. We also observed anti-Sm titers rise and subsequently fall in a patient with severe flare and aggressive immunosuppressive treatment respectively. These data may suggest that anti-Sm antibodies are produced by plasmablasts rather than plasmacells on at least some occasions and thus be amenable to suppression by treatment. Larger studies will be needed to further support these findings
To cite this abstract in AMA style:
Megaris F, Wu E, Kirou K. Anti-Sm Antibody Titers Vary During SLE Disease Course [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/anti-sm-antibody-titers-vary-during-sle-disease-course/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-sm-antibody-titers-vary-during-sle-disease-course/