Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Neuropsychiatric systemic lupus erythematosus (NPSLE) can involve the central (CNS) and peripheral nervous system (PNS). Several autoantibodies have been associated with CNS NPSLE including anti-phospholipid, anti-ribosomal P and anti-NMDA receptor 2; however, there are no known autoantibodies specifically associated with PNS involvement. M-Phase Phosphoprotein 1 (MPP1; also known as kinesin family member 20B, KIF20B) is a protein involved in cytokinesis and anti-MPP1 autoantibodies have been associated with idiopathic ataxia. We examined the frequency of anti-MPP1 and its demographic and clinical associations including CNS and PNS NPSLE in our local SLE cohort.
Methods: Patients fulfilled the ACR or SLICC classification criteria (CC) for SLE. Age, sex, race, SLEDAI-2K, SLICC CC, and sera were collected at the time of enrolment and up to two follow up visits. NPSLE events fulfilling the ACR case definitions were identified from date of SLE diagnosis by medical record review. Anti-MPP1 titers were determined by an addressable laser bead immunoassay (ALBIA) utilizing a purified recombinant protein. ALBIA results were expressed as median florescence units (MFU). A dilution of ≥1:500 MFU was considered positive. Chi-squared and t-tests were performed to compare demographic and clinical characteristics, including NPSLE manifestations, between patients who were ever anti-MPP1 positive (MPP1+) vs those who were never positive (MPP1-). Multivariable logistic regression analysis was used to determine associations between MPP1+ and variables that were statistically significant in the univariable analysis (p < 0.05).
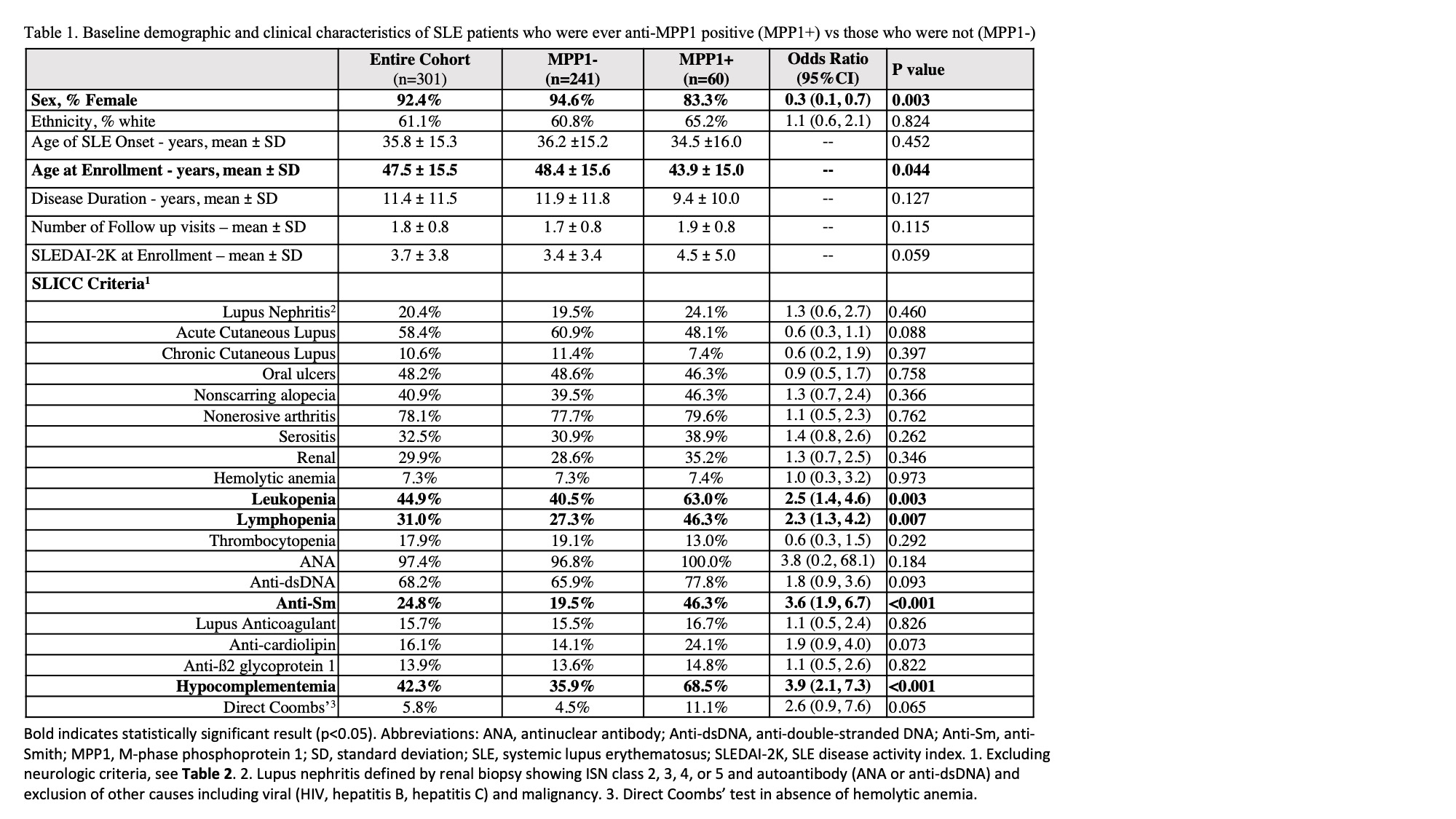
Results: Of the 301 SLE patients studied (mean disease duration 11.4 ± 11.5 years), 19.9% were MPP1+. When compared to MPP1- patients, MPP1+ patients had a lower proportion of females (OR 0.3, 95% CI 0.1-0.7), were younger at enrolment (43.9 ± 15.0 years vs 48.4 ± 15.6 years; p=0.04), had more leukopenia (OR 2.5, 95% CI 1.4-4.6), lymphopenia (OR 2.3, 95% CI 1.3-4.2), anti-Sm antibodies (OR 3.6, 95% CI 1.9-6.7) and hypocomplementemia (OR 3.9, 95% CI 2.1-7.3) (Table 1). 72.4% of patients met criteria for any NPSLE manifestation with no difference between MPP1+ and MPP1- patients (Table 2). When PNS NPSLE manifestations were examined, patients with any peripheral neuropathy (OR 3.2, 95% CI 1.7-6.2), mononeuropathy (OR 8.7, 95% CI 2.1-36.0), and cranial neuropathy (OR 6.5, 95% CI 2.5-17.0) were more likely to be MPP1+. Multivariable analysis demonstrated that any peripheral neuropathy (OR 4.8, 95% CI 2.2-10.8) and cranial neuropathies remained significantly associated with MPP1+ (OR 9.7, 95% CI 2.9-32.2) (Table 3).
Conclusion: Anti-MPP1 may be an important biomarker for peripheral neuropathies, in particular, cranial neuropathies in SLE. These findings are being validated in a larger, multicentre SLE cohort.
To cite this abstract in AMA style:
Krustev E, Buhler K, Cardwell F, Fritzler M, Clarke A, Choi M. Anti-MPP-1 Autoantibodies in Systemic Lupus Erythematosus: A Potential Biomarker for Neuropsychiatric Manifestations [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/anti-mpp-1-autoantibodies-in-systemic-lupus-erythematosus-a-potential-biomarker-for-neuropsychiatric-manifestations/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-mpp-1-autoantibodies-in-systemic-lupus-erythematosus-a-potential-biomarker-for-neuropsychiatric-manifestations/