Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose : Clinically amyopathic dermatomyositis (CADM) is a subset of dermatomyositis (DM) presenting with the characteristic rash(es) of DM without objective muscle weakness. Asian studies report that anti-MDA5 autoantibody (autoAb) in CADM is associated with interstitial lung disease (ILD), particularly rapidly-progressive ILD (RPILD). These associations have not been established in U.S. myositis patients. The goals of our study were to determine the association of anti-MDA5 autoAb with ILD, RPILD and survival in U.S. patients with CADM and DM.
Methods: A cohort of CADM patients were matched (gender and age) 1:1 with classic DM controls. CADM was defined by a DM rash without objective muscle weakness for at least 6 months after rash onset with no or minimal abnormalities of serum muscle enzymes, electromyography or muscle biopsy. We collected clinical, laboratory, radiographic and survival data on the CADM and DM cohorts. Anti-MDA5 autoAb was measured by serum ELISA on both groups. ILD was defined by fibrosis on imaging studies and RPILD by the acute onset and rapid worsening of dyspnea or severe radiographic ILD/fibrosis within 3 months from the onset of respiratory symptoms. Kaplan-Meier and Cox proportional hazard model was used for survival analysis. Chi-square test and Student’s t-test was used for other associations.
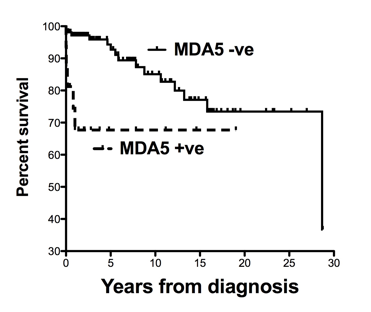
Results: We identified 61 CADM patients and 61 age and gender matched DM controls. There were 62% and 64% females, 92% and 87% Caucasians, with a mean (SD) age of 48.2 (16.9) and 44.8 (17.6) in the DM and CADM cohorts, respectively. Anti-MDA5 frequency was similar in CADM (13.1% [8/61]) and DM (13.1% [8/61]) as was ILD (CADM: 31.1% [19/61], DM: 26.2% [16/61]) or RPILD (CADM: 8.2% [5/61], DM: 5% [3/61]), p = NS]. Anti-MDA5 positivity was significantly associated with ILD as 50% (8/16) of MDA-5+ subjects had ILD vs. 25.5% (27/106) of MDA-5- subjects (p=0.043). Anti-MDA5 was strongly associated with RPILD (p<0.001). Among 8 anti-MDA5+ patients with ILD, 7 had RPILD leading to early death in 5; whereas, only one MDA5- patient had RPILD (1/106). Anti-MDA5 positivity was significantly associated with poor survival (Figure 1, p=0.007), but the presence of ILD or CADM was not predictive of survival. RPILD had a very poor prognosis with hazard ratio (HR) of 28 (CI: 9-86, p <0.001). Multivariate analysis suggested that anti-MDA5 positivity predicted survival (HR [C.I.] = 7 [2-23], p=0.001) even after controlling for diagnosis (CADM vs. DM), age at diagnosis, gender, ethnicity, smoking, and ILD (p=0.002).
Conclusion: CADM is not associated with anti-MDA5 or ILD in U.S. DM patients. Anti-MDA5 has a similar frequency in CADM and DM and is significantly associated with ILD, RPILD, and poor survival in U.S. DM patients.
Figure 1. Kaplan-Meier survival curve for anti-MDA5 positive and negative patients (p-value=0.007).
Disclosure:
S. Moghadam-Kia,
None;
C. V. Oddis,
Novartis Pharmaceutical Corporation,
5;
S. Sato,
Holding a patent on anti-MDA5 antibody-measuring kit,
7;
M. Kuwana,
Holding a patent on anti- MDA5 antibody-measuring kit. ,
7;
R. Aggarwal,
Questcor, Pfizer,
2,
Questcor, ATry pharma,
5.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-mda5-is-associated-with-rapidly-progressive-interstitial-lung-disease-and-poor-survival-in-u-s-patients-with-amyopathic-and-myopathic-dermatomyositis/