Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) with rheumatoid arthritis (RA) has been reported rarely, and, studies have found ANCA positivity in RA. The objective of the study was to describe a cohort of patients with RA and AAV and to compare patients with RA+AAV to those with RA+ANCA positivity without AAV.
Methods: In this retrospective study, a cohort of patients with RA+ANCA positivity evaluated at an academic center were included. Data abstracted included demographics, seropositivity, ANCA specificity, clinical characteristics of RA, diagnosis of AAV and clinical features of AAV.
Results: The study included 77 patients, mean (±SD) age 60.2 (17.2) years, 78% female. ANCA serologies included perinuclear (p)-ANCA in 58%, cytoplasmic (c)-ANCA in 26%, myeloperoxidase (MPO) in 43% and proteinase 3 (PR3) in 26%. Twenty patients (26%) were p-ANCA/MPO positive, 3 patients (4%) c-ANCA/PR3 positive, 7 patients (9%) were p-ANCA/PR3 positive and 1 patient (1%) was c-ANCA/MPO positive.
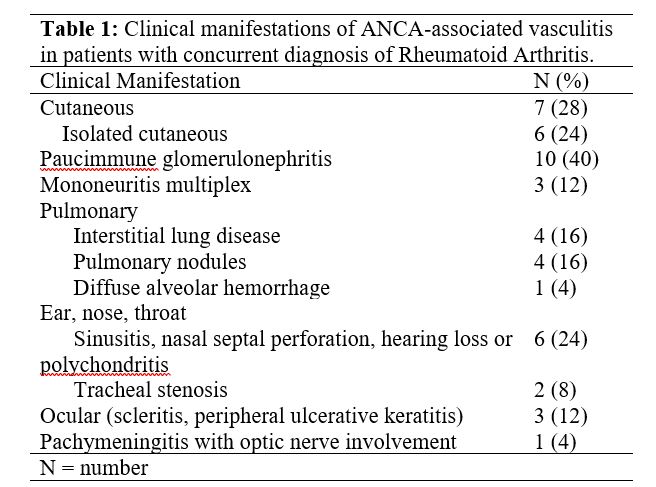
Twenty-five patients (32%) had a diagnosis of AAV; 9 (36%) microscopic polyangiitis (MPA), 8 (32%) granulomatosis with polyangiitis (GPA), 1 (4%) eosinophilic granulomatosis with polangiitis (EGPA), 1 (4%) GPA versus rheumatoid vasculitis (peripheral ulcerative keratitis, scleritis, sudden hearing loss, MPO positive). In 6 patients (24%) diagnosis was unclassifiable (1 interstitial lung disease attributed to vasculitis, 3 cutaneous vasculitis with ulcerations, 1 case of multiple digital infarctions from vasculitis, 1 leukocytoclastic vasculitis). Diagnosis of RA preceded vasculitis in 92% cases, was concurrent in 4% and followed vasculitis in 4%. Clinical manifestations of AAV are in Table 1. Among patients with RA+ANCA positivity but no diagnosis of AAV, 1 patient had nasal septal perforation with polyposis, 1 patient had vasculitic rashes and neuropathy attributed to vasculitis from RA, 2 patients had retinal vasculitis.
A comparison of patients with RA+AAV, and, patients with RA+ANCA without AAV is in Table 2. A higher proportion of patients with ANCA positivity via indirect immunofluorescence (IIF) along with antibody specificity to MPO or PR3 had a clinical diagnosis of AAV. These findings remained significant even if the 6 patients with unclassifiable disease were excluded (data not shown).
Conclusion: AAV in RA included an even number of cases of GPA and MPA. The diagnosis of RA almost always preceded the diagnosis of AAV and renal involvement was the most commonly present manifestation of AAV. There was uncertainty regarding attribution of isolated cutaneous vasculitis to RA or AAV and 24% of this cohort diagnosed as AAV had isolated skin disease. Many patients without vasculitis had positive MPO or PR3 antibodies. The presence of ANCA via IIF with MPO or PR3, even if discordant, separated patients with RA+AAV from those without vasculitis highlighting the need for clinical vigilance in this subset of patients with RA. The immune mechanisms underlying this rare overlap need to be elucidated.
To cite this abstract in AMA style:
O'Brien C, Ranganath V, Kermani T. ANCA Positivity and ANCA Associated Vasculitis in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/anca-positivity-and-anca-associated-vasculitis-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anca-positivity-and-anca-associated-vasculitis-in-patients-with-rheumatoid-arthritis/