Session Information
Date: Sunday, November 17, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Kawasaki disease (KD) is a systemic vasculitis, typically affecting young children, and is the leading cause of acquired heart disease in children in developed countries. Adult-onset KD is rare and often misdiagnosed or diagnosed late [1]. There is a scarcity of national population studies on hospitalizations of adult patients with KD. We aim to study reasons for hospitalization, baseline demographic characteristics, and outcomes of hospitalizations of adult patients with KD.
Methods: Data were abstracted from the National Inpatient Sample (NIS) 2016 and 2017 combined database. NIS is a nationally representative approximate 20-percent stratified sample of all discharges from U.S community hospitals, excluding rehabilitation and long-term acute care hospitals. The numbers in the databases are weighted to optimize national estimates. Each hospitalization in the NIS has only 1 principal diagnosis and can have up to 39 secondary diagnoses. The principal diagnosis is the main reason for hospitalization. Any diagnosis other than the principal, is a secondary diagnosis. The NIS was searched for hospitalizations for adult patients aged ≥ 18 years with a diagnosis of KD as the principal or secondary diagnosis using International Classification of Diseases, tenth revision (ICD-10) code “M303”. Baseline demographic characteristics and outcomes of these hospitalizations were recorded. Analyses were performed using STATA,16. We used a “rank” order command in STATA to arrange the most common reasons for hospitalization in descending order of frequency based on ICD-10 code organ system categories and the most specific ICD-10 code principal discharge diagnosis.
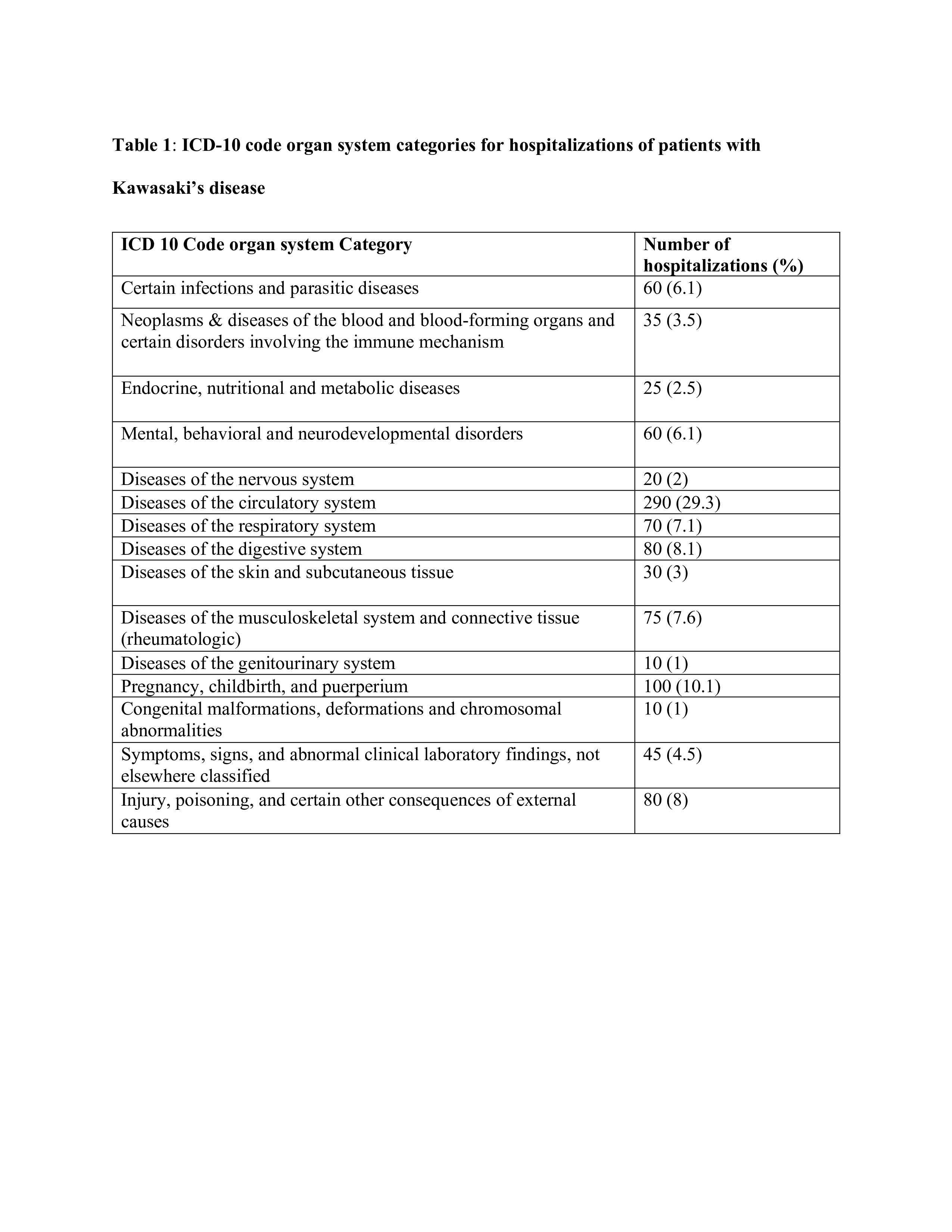
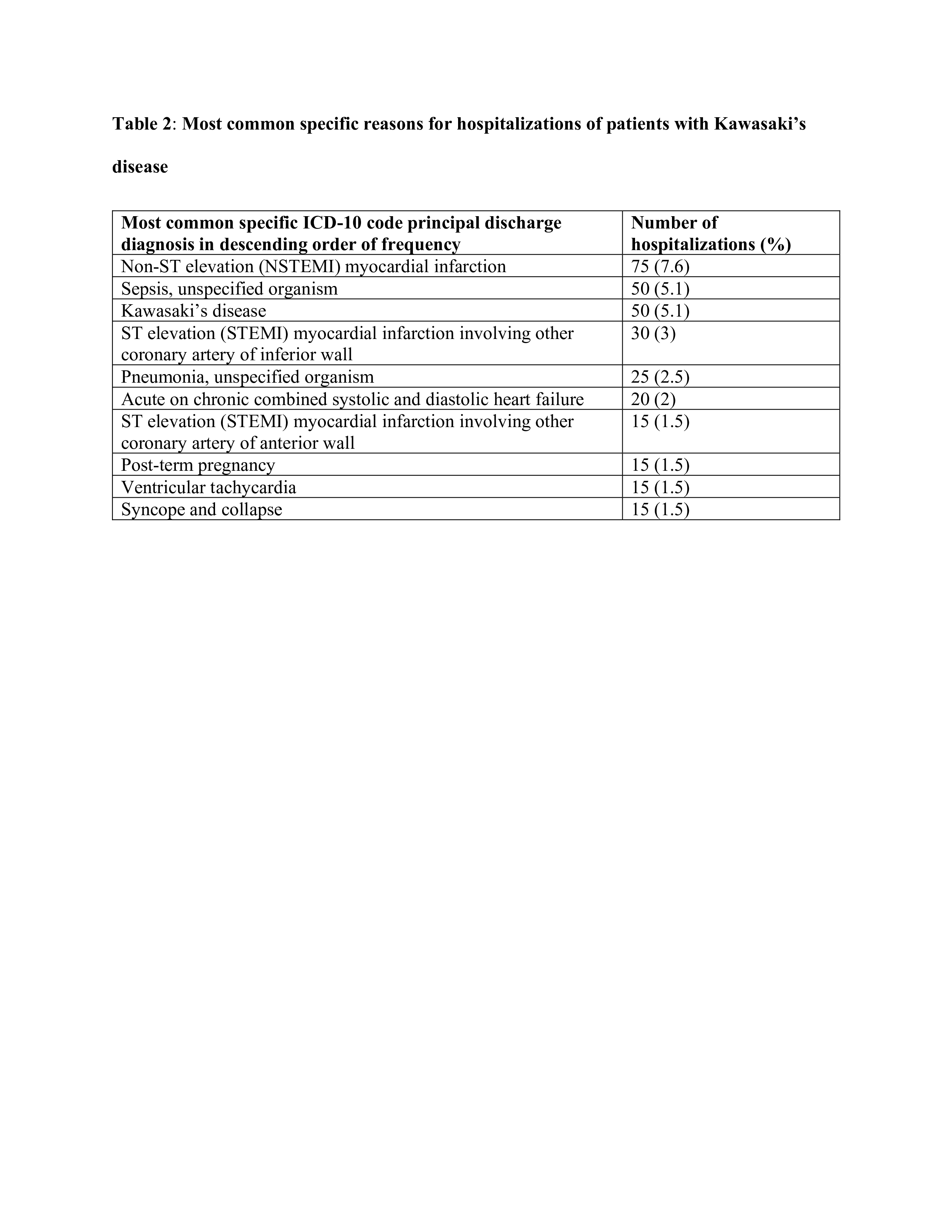
Results: There were over 70 million discharges included in the 2016 and 2017 combined NIS database. We found 11,355 hospitalizations with either principal or secondary diagnosis of KD. Out of these, 990 hospitalizations were for adult patients. Adult KD hospitalizations were mostly males (58%), mean age of 41 years, whites (58.9%), privately insured (43.9%), and presented to teaching hospitals (71.2%). Inpatient mortality occurred in 2%, mean hospital length of stay was 5.5 days, and mean total hospital charges was 74,816 U.S dollars. Cardiovascular (CV) diseases were the most common reason for hospitalization by ICD-10 code category; 290 (29.3%) (Table 1). Non-ST elevation myocardial infarction (NSTEMI) was the most common specific reason for hospitalization; 75 (7.6%) ( Table 2) , followed by sepsis, unspecified organism 50 (5.1%), and KD 50 (5.1%).
Conclusion: CV diseases were the most common reason for hospitalization by ICD-10 code category in adult patients with KD. NSTEMI, sepsis, and KD were the top 3 most common specific reasons for hospitalization. Optimal management of KD and associated CV comorbidities, early detection, and management of infections in the outpatient setting are important in reducing hospitalizations of these patients.
To cite this abstract in AMA style:
Mamoh U, Salia S, Morny J, Odion J, Ewuru E, Onobraigho P, Omoike E, Ijioma O, Ezomo O, Edigin E. Analysis of Hospitalizations of Adult Patients with Kawasaki’s Disease: A United States Population Based Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/analysis-of-hospitalizations-of-adult-patients-with-kawasakis-disease-a-united-states-population-based-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-hospitalizations-of-adult-patients-with-kawasakis-disease-a-united-states-population-based-study/