Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Non-infectious uveitis (NIUs) encompass a varied group of inflammatory diseases affecting the uvea and adjacent tissues, with evidence suggesting an immune-mediated cause. A correct management of these conditions is essential to prevent visual loss and the development of ocular complications. Although immunosuppressive drugs (ISDs) have shown effectiveness in achieving a sustained control of the inflammatory process, not all patients achieve a satisfactory response.
To identify factors affecting the response rate to ISDs in subjects with NIUs.
Methods: Longitudinal retrospective study, with patients collected from the Hospital Clinico San Carlos Uveitis Clinic, included from 1991 until December 2018, and followed-up until December 2019. Patients entered the study at ISD prescription and were followed-up until a) the achievement of a good therapeutic response (GTR), b) ISD treatment change (withdrawal of the prescribed ISD and/or addition of a new ISD), c) 12 months of follow-up, or d) loss of follow-up or end of the study (December 31th, 2019). GTR was defined as the complete resolution of the eye inflammatory manifestations and oral corticosteroid ≤10 mg of prednisone equivalent a day. Furthermore, this situation had to be maintained in at least two consecutive visits spanned at least 28 days. KaplanMeier (KM) curves were set to account for GTR. Associated demographic, clinical and treatmentrelated factors were analyzed using bivariate and multivariate Cox robust regression models. Different models were compared using the Akaike Information Criteria, to select the fittest model to the data. Proportional hazard assumption was tested using Schoenfeld residuals and the scaled Schoenfeld residuals. In case a variable or certain category of a categorical variable were nonproportional, they were included in the Cox models with a time-varying effect, in case the interaction with time was significant (p< 0.05).
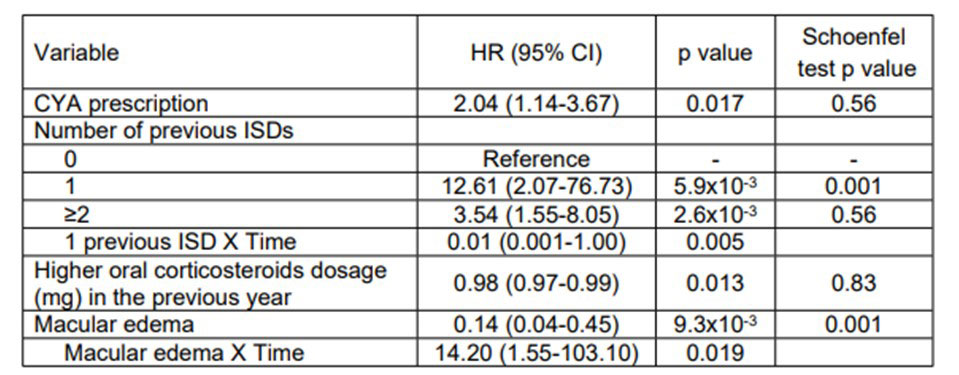
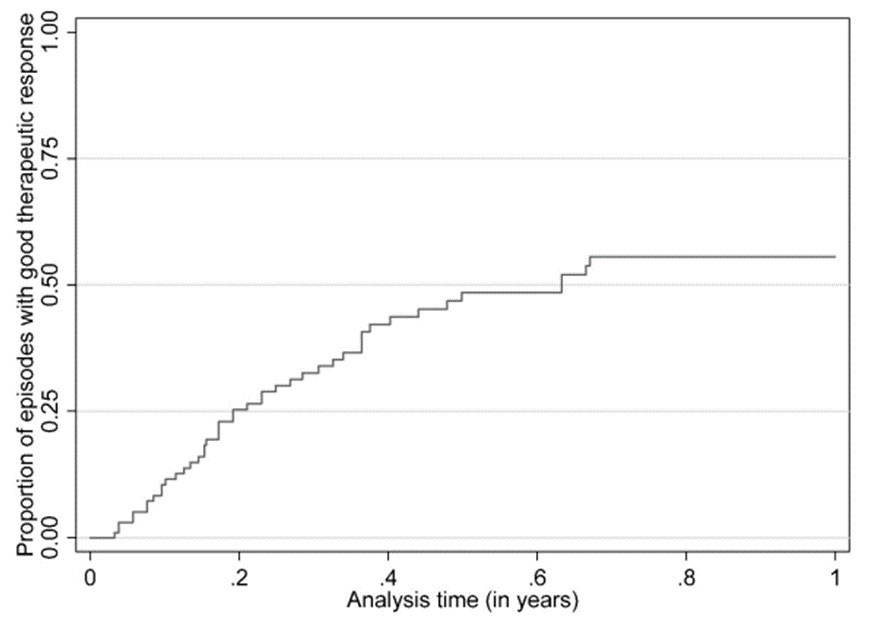
Results: 73 patients (100 episodes of ISD prescription) were analyzed. In 44 episodes, a GTR was achieved (incidence rate 102.0 [95% Confidence Interval (CI): 75.9 to 137.1] per 100 patient-years). Figure 1 shows the KM curve for GTR. In the bivariate analysis, several variables showed a significant association with GTR, including gender, diagnosis of Behçet Disease, prescription of Cyclosporine A (CYA), number of previously prescribed ISDs, previous use of the same ISD, previous discontinuation of a ISD due to inefficacy, higher systemic corticosteroid use in the previous year before ISD prescription, presence of macular edema (ME), and longer intermediate and posterior activity before ISD prescription. Table 1 shows the results of the multivariate analysis. Prescription of CYA was associated with a higher hazard of GTR, compared with the use of other ISDs (methotrexate, azathioprine or biologic drugs). In addition, the higher dosage of oral corticosteroids used in the previous year before ISD prescription, the lower the hazard of achieving a GTR. Finally, presence of ME at prescription was associated with lower hazard of GTR, although this risk diminished with time.
Conclusion: We have identified several variables associated with therapeutic response to ISDs in NIUs patients.
To cite this abstract in AMA style:
Álvarez Hernández M, Gómez Gómez A, Borrego Sanz L, Méndez Fernández R, Arriola Villalobos P, Pato Cour E, Díaz Valle D, Rodriguez-Rodriguez L. Analysis of Factors Associated with Good Therapeutic Response to Immunosuppressive Drugs in Patients with Non-infectious Uveitis: A Survival Analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/analysis-of-factors-associated-with-good-therapeutic-response-to-immunosuppressive-drugs-in-patients-with-non-infectious-uveitis-a-survival-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-factors-associated-with-good-therapeutic-response-to-immunosuppressive-drugs-in-patients-with-non-infectious-uveitis-a-survival-analysis/