Session Information
Date: Monday, November 9, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Bench to Bedside
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Cognitive dysfunction (CD) is very prevalent in SLE and significantly affects quality of life. Altered functional brain mechanisms are associated with CD in SLE. We previously used functional magnetic resonance imaging (fMRI) to show altered mechanisms in the Default Mode Network (DMN), a network involved in self-reflection and is acquiescent during cognitive tasks. In this study, we examined the effects of disease activity on functional connectivity (FC) within the DMN using resting state (rs) fMRI. We hypothesised that those with SLE, and specifically those with active disease, would have reduced FC within the DMN compared to healthy controls.
Methods: 19 SLE-active (SLE-F) and 23 SLE-stable (SLE-S) all meeting 1997 ACR or SLICC criteria and 30 healthy controls (HC) were recruited. In the SLE participants, active disease was defined as BILAG A or B with a change in treatment. Stable disease was defined as SLEDAI-2K ≤4. Demographic, clinical and psychiatric data were collected for all participants. A T2-weighted scan was undertaken and reviewed by a neuroradiologist to provide a Scheltens score for brain abnormalities. A T2*-weighted rsfMR scan was acquired. These images, after preprocessing, were analysed using independent component analysis (ICA). Fischer’s z-scores were extracted from those temporospatial nodes associated with the DMN and entered into ANOVAs or Kruskal-Wallis tests.
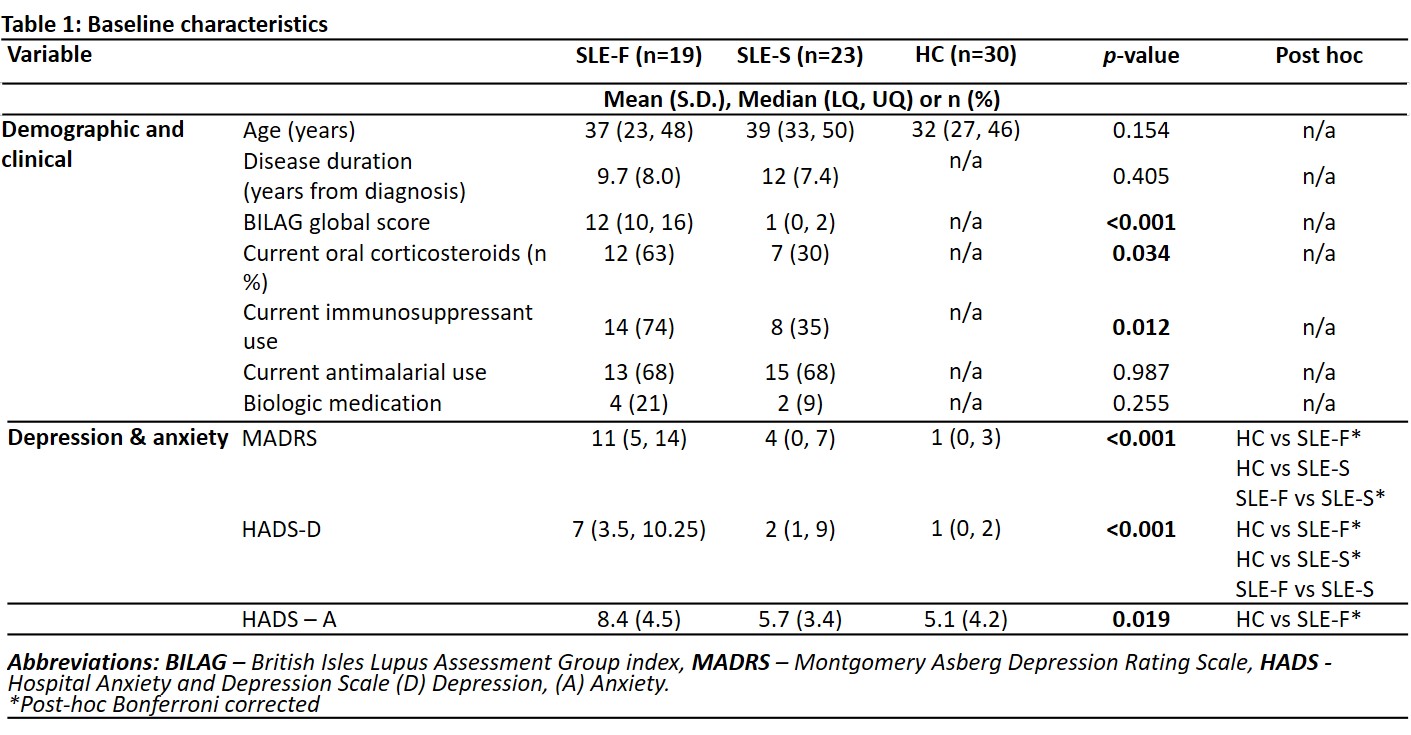
Results: Participants were well matched on key demographics. Significant differences were found between the SLE groups on factors associated with disease activity and psychological factors (Table 1).
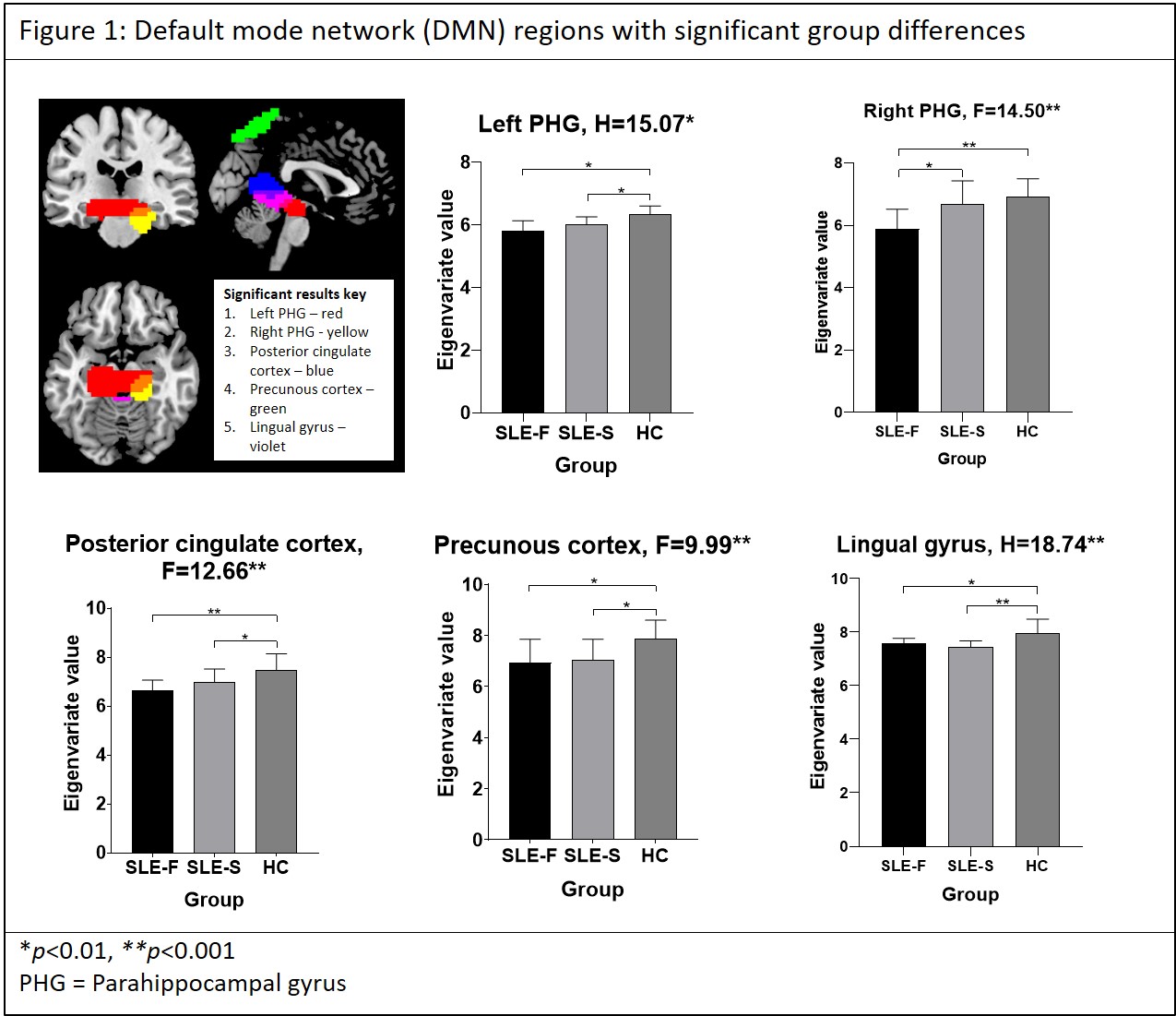
14 DMN nodes were defined using ICA. Significant group differences (p< 0.001) were found in five of the nodes: precunous cortex, right parahippocampal gyrus (PHG), posterior cingulate cortex, lingual gyrus and left PHG. In all regions, except the right PHG, the SLE groups had reduced FC compared to the HC group. In the right PHG the SLE-F group had reduced FC compared to the other two groups (Figure 1).
Correlations comparing the significant nodes with Scheltens score and depression and anxiety measures for the SLE groups combined were undertaken. Depression score (MADRS) was negatively correlated with FC in both the left and right PHG (rs=-0.476, p=0.001 and rs=-0.494, p=0.001, respectively).
Conclusion: Altered FC was evident in DMN nodes for SLE groups irrespective of disease activity. Reduced FC in these areas could be indicative of fatigue. The inability to “switch off” the DMN during cognitive tasks may impact the FC of the DMN in SLE. The DMN is involved in self-reflective processes and altered FC is associated with major depression. Our SLE groups had higher, but not clinically significant, depression scores compared to HC and our correlations found altered FC associated with depression scores. When considering rsfMRI as a potential marker for CD in SLE other contributing factors, such as depression, must also be considered.
To cite this abstract in AMA style:
Barraclough M, McKie S, Parker B, Jackson A, Elliott R, Bruce I. Altered Brain Functional Connectivity in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/altered-brain-functional-connectivity-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/altered-brain-functional-connectivity-in-systemic-lupus-erythematosus/