Session Information
Date: Saturday, November 12, 2022
Title: Vasculitis – ANCA-Associated Poster I: Epidemiology, Outcomes, and Classification
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: Despite improvement in treatment and early diagnosis of ANCA-associated Vasculitis (AAV), mortality remains elevated. Early deaths in AAV patients are often attributed to the vasculitis and infections secondary to treatment. The purpose of this study was to investigate excess mortality and cause-specific deaths in patients with AAV compared to the general population.
Methods: Using the Swedish National Board of Health and Welfares database on cause of death we investigated all cause and cause-specific mortality in two large population-based cohorts of AAV. Patients with AAV from two defined geographic areas in Sweden diagnosed between 1997 and 2019 were included in this study. All diagnoses were confirmed by case record review. Patients were classified into granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) and eosinophilic GPA (EGPA) by using the European Medicine Agency algorithm. For each patient with AAV, 20 controls were selected from the background population matched for age, sex, and place of residency. Controls with a vasculitis diagnosis were excluded. Data on all-cause mortality were extracted from the cause of death database and were returned as one or more ICD-codes (10th version), where one diagnosis was deemed underlying and the others as contributing in a chain that lead to death. The chain of ICD-codes that lead to death were specified by the physician that pronounced the death. Person-year time of follow-up was calculated from the date of AAV diagnosis for cases (index-date for controls) to death or end of study (December 31, 2020). Rate of death for patients and controls was calculated and rate ratio (death rate in AAV: controls) were estimated. Survival was studied using the Kaplan Meier curves and Log Rank tests. Primary cause of death was grouped into the following categories: vasculitis, infection, cardiovascular, cancer and other.
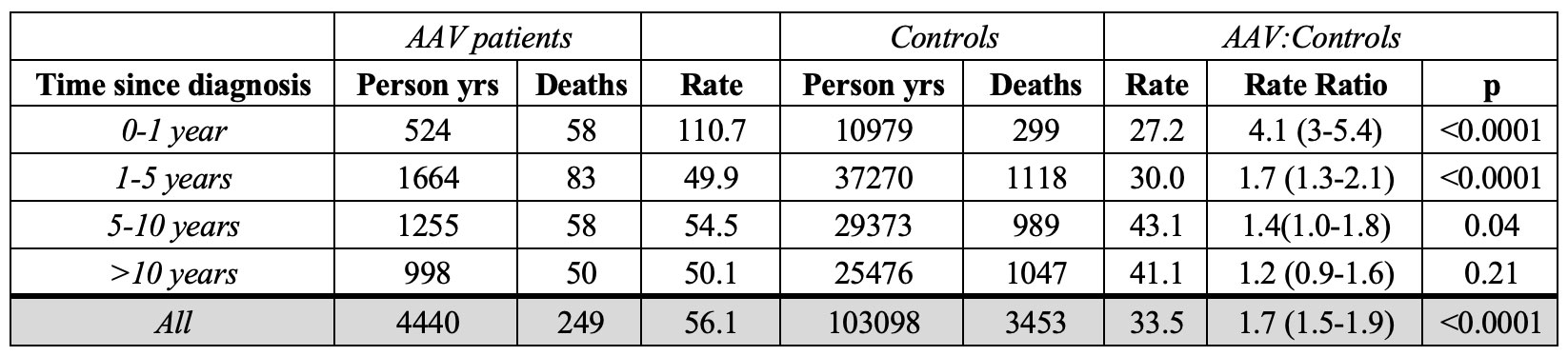
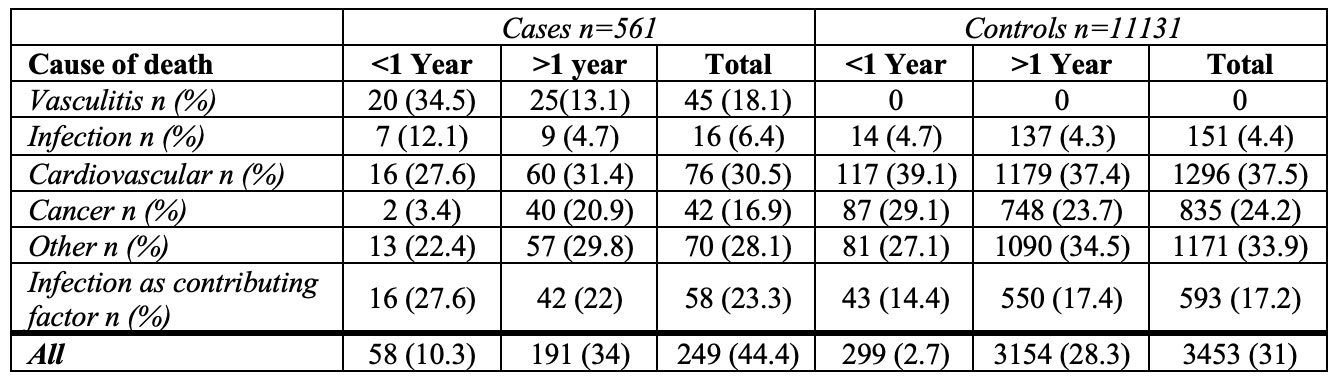
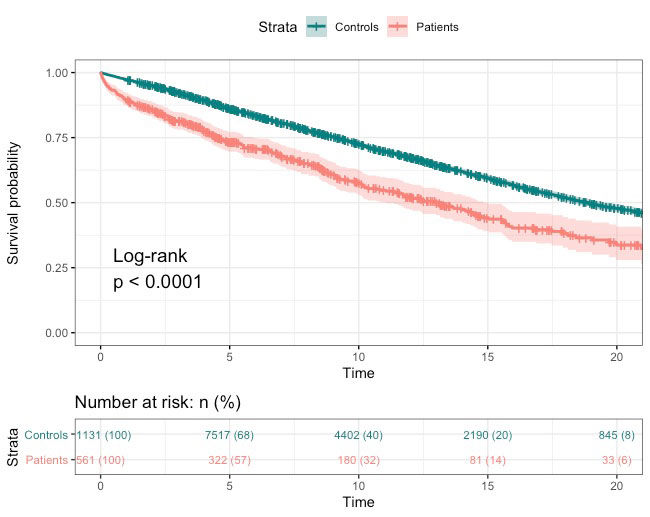
Results: A total of 561 patients and 11131 controls were included. Patients were classified as: GPA 290, MPA 248 and EGPA 23. 288 (51%) patients were PR3-ANCA positive and 243 (43%) were MPO-ANCA positive. Two hundred and forty-nine patients died during 4440 years of follow up vs. 3453 controls during 103098 years of follow up. The rate of death was 56.1/1000 person-year (py) in AAV patients vs. 33.5/1000 py in controls resulting in a rate ratio of 1.7 (95% CI 1.5-1.9), Table 1. The 1, 5 and 10-years cumulative survival was 90%, 73% and 57% in patients and 97%, 86% and 73% in controls (p < 0.0001), Figure 1. During the first year from diagnosis, the main cause of death was vasculitis, cardiovascular and other in patients vs. cardiovascular, other and cancer in controls, Table 2). Infection was a contributing factor to death in 28% of deaths in patients and 19% in controls.
Conclusion: There is a significant excess mortality in patients with AAV compared to matched controls.
Death rate is higher in the first year after diagnosis and remains elevated in long-term follow up. The proportions of specific causes of death differ from the matched controls with vasculitis dominating as primary cause of death in the first year after diagnosis.
To cite this abstract in AMA style:
Wilding A, Weiner M, Rathmann J, Segelmark M, Mohammad A. All-Cause and Cause-Specific Mortality in ANCA-Associated Vasculitis: A Population-based Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/all-cause-and-cause-specific-mortality-in-anca-associated-vasculitis-a-population-based-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/all-cause-and-cause-specific-mortality-in-anca-associated-vasculitis-a-population-based-study/