Session Information
Date: Sunday, November 12, 2023
Title: (0176–0195) Healthcare Disparities in Rheumatology Poster I: Lupus
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) care and outcomes are associated with significant racial and socioeconomic disparities in the US, particularly among young Black and Hispanic/Latina women. We previously identified disparities, including gaps in SLE retention in care (defined as a rheumatology clinic visit or lupus-specific lab test every 6 months) and hydroxychloroquine (HCQ) use and adherence. We sought to address these modifiable gaps in SLE care by adapting intervention approaches from other chronic diseases. We engaged patients and healthcare community stakeholders to garner input to prioritize actionable steps and intervention strategies to reduce disparities in SLE retention in care and HCQ use to improve outcomes and equity.
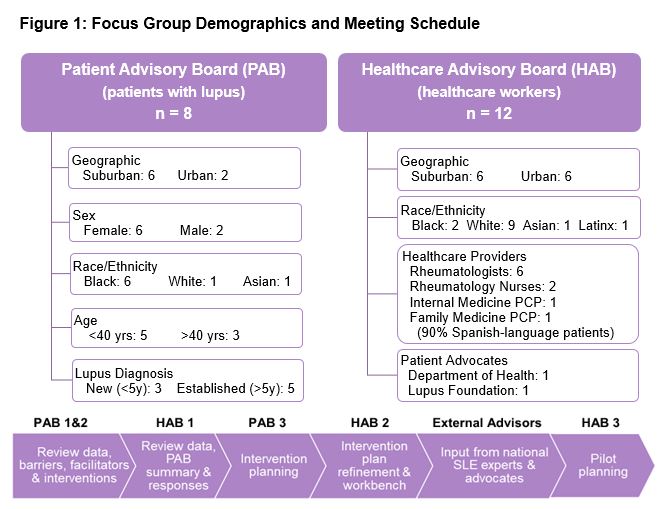
Methods: We recruited SLE experts and stakeholders, including patients, providers, and advocates (State Public Health Department, Lupus Foundation, and the American College of Rheumatology) to adapt intervention strategies from other chronic conditions to be tested in SLE. The patient advisory board (PAB; n=8) included patients with SLE representing racial, geographic, age, and sex diversity (Figure 1). PAB insights were presented to a healthcare advisory board (HAB; n=12) of 6 rheumatologists, 2 rheumatology nurses, 2 primary care providers, and 2 patient advocates (Figure 1). The HAB reviewed prior findings on SLE care gaps and evaluated proven interventions for a pilot. Each group had 3 virtual meetings of 90 minutes (total=6) scheduled to be alternating and iterative. Sessions were audio-video recorded and analyzed using direct content analysis with NVivo software (Melbourne, AU).
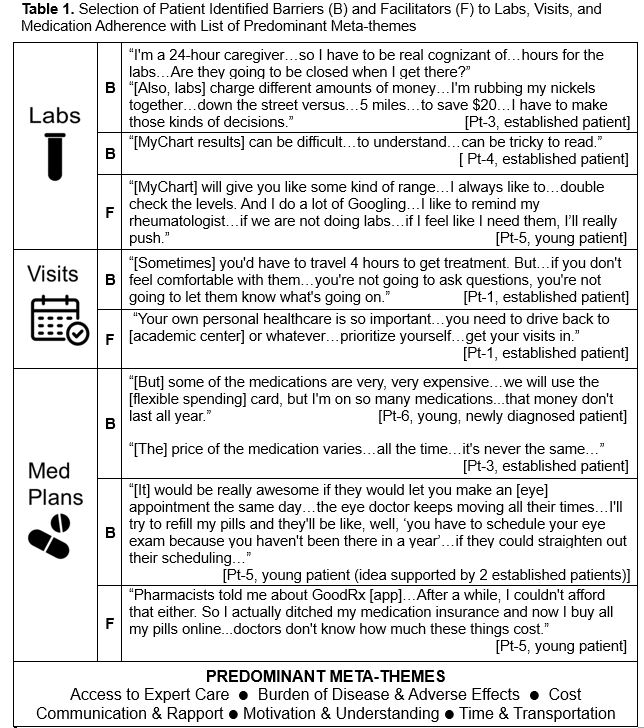
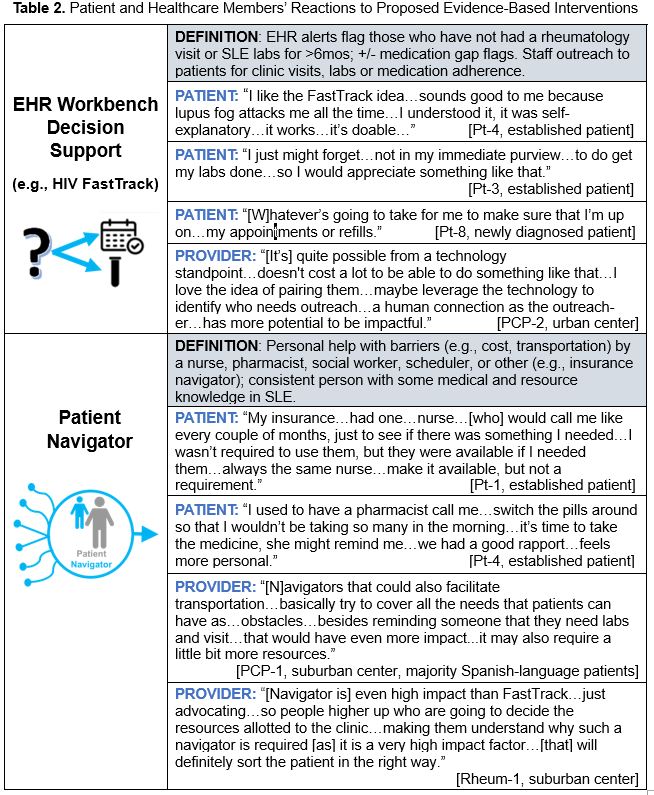
Results: The PAB discussed several barriers to SLE retention in care and HCQ, categorized as: labs, visits, and medication adherence (see Table 1 quotes and meta-themes). Facilitators were similarly identified and grouped (Table 1). The main evidence-based interventions considered were electronic health record (EHR) workbench decision support (e.g., HIV FastTrack) that cues staff action upon missed visits and labs; shared decision making; and patient navigators (Table 2). All HAB members and 5 of 8 PAB members supported implementing EHR workbench decision support. PAB and HAB members also suggested including a patient navigator as a supplement to answer patient questions and address challenges in scheduling, medication dosing, and cost barriers, among others. Among HAB members, 8 of 12 recommended EHR workbench decision support as high-impact and low-effort; while 7 of 12 rated patient navigator as high-impact but high-effort. Many discussed that the two could be complementary, recommending EHR workbench decision support first, followed by patient navigator. Indicators for additional support recommended by HAB members were social determinants of health, missed labs or clinic visits, and frequent acute care.
Conclusion: Patient and healthcare stakeholders endorsed implementing EHR workbench decision support, potentially followed by a patient navigator, to reduce disparities and care gaps in SLE. An external advisory board of national SLE leaders is advising scalability for a larger study, and the findings will inform addressing key gaps and unique factors in SLE.
To cite this abstract in AMA style:
Parikh S, Messina M, Garg S, Ferguson S, Ramly E, Gilmore-Bykovskyi A, Phelps K, Bartels C. Advancing Health Equity with Lupus Stakeholders to Close Care Gaps and Disparities [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/advancing-health-equity-with-lupus-stakeholders-to-close-care-gaps-and-disparities/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/advancing-health-equity-with-lupus-stakeholders-to-close-care-gaps-and-disparities/