Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Transitioning from pediatric to adult rheumatology care around age 18 is an important and often challenging period in patients’ lives. Differences between adult and pediatric care and patient-related factors (including psychosocial concerns) represent some potential challenges and barriers to a successful transition. These barriers can lead to gaps in care and loss to follow-up after transfer to adult care. In contrast to pediatricians and pediatric trainees who are familiar with adolescent behavior and psychosocial concerns, adult rheumatologists report inadequate training in transition issues, specifically psychosocial concerns, and are less familiar with transition recommendations and guidelines. The purpose of this study was to assess the comfort level, current practices, and barriers to provision of optimal transition care faced by adult rheumatologists in supporting young adults with rheumatic conditions in Canada.
Methods: Questions were informed by a previous study (Zisman et al, 2020) and milestones listed by the Royal College of Physicians and Surgeons of Canada for the Entrustable Professional Activities (EPAs) applicable to care for patients transitioning to adult practice. Feedback during questionnaire development was obtained from the Canadian Rheumatology Association (CRA) Transition Working Group prior to finalizing survey questions. The survey was electronically distributed to adult rheumatologists and adult rheumatology trainees via the CRA over a period of four months from December 2021-March 2022.
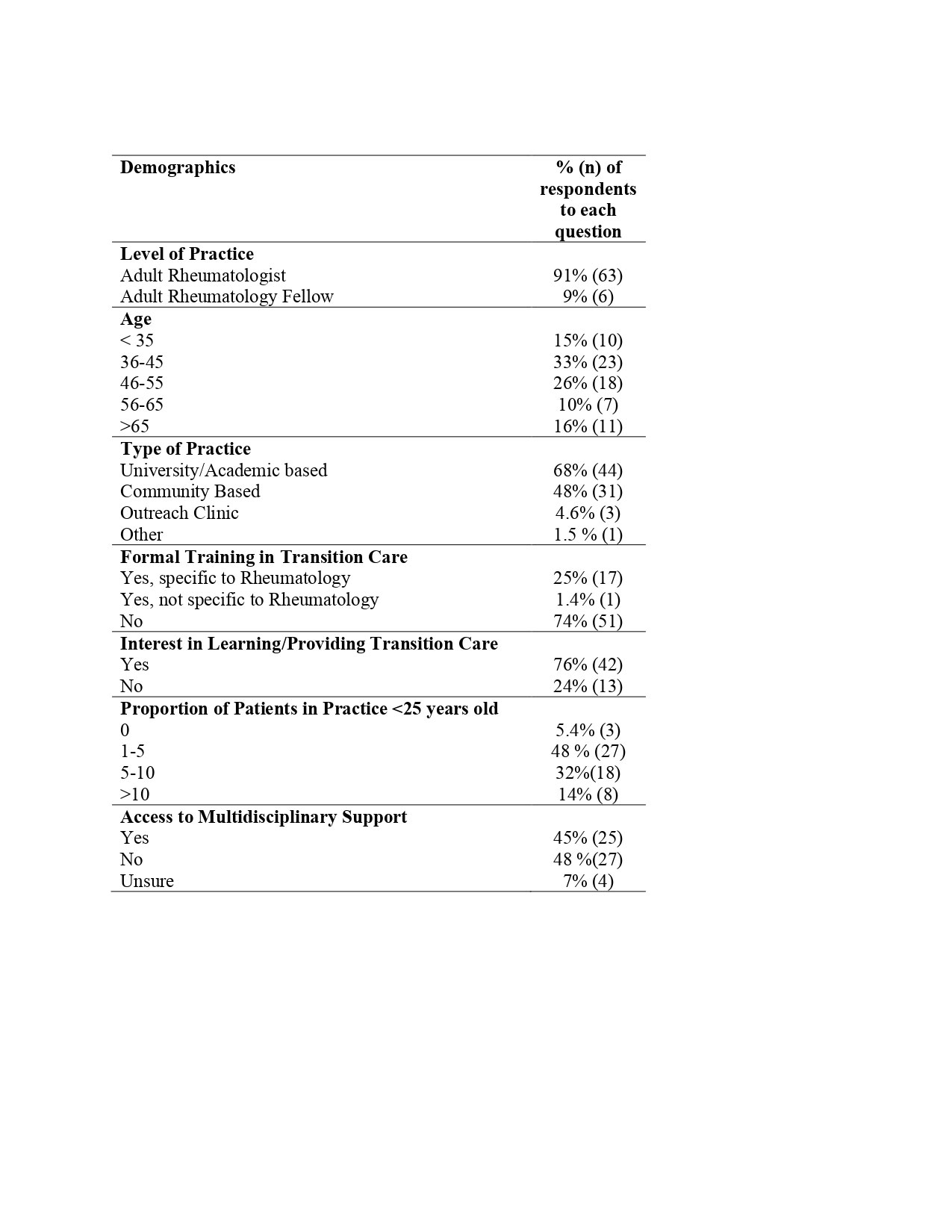
Results: A total of 451 physicians received the survey and 15.2% responded. Most rheumatologists were from Ontario and had spent >10 years in practice. A lack of training in transition care was reported by 75%, although the same proportion were interested in learning more about providing care to young adults (Table 1). Approximately 40% of respondents felt comfortable discussing psychosocial concerns such as gender identity, sexuality, contraception, drug and alcohol use, vaping, and mental health. However, 45-50% reported not discussing vaping or gender identity at all compared to the other topics where there was more frequent discussion with patients. The majority of respondents felt that the family physician should be the health care provider to address these topics. The most frequently reported barriers to providing transition care were lack of primary care providers (66%), allied health support (72%), time (57%) and training in caring for this age group of patients (49%).
Conclusion: Most adult rheumatologists lack formal training in transition care and view this gap in knowledge as a barrier to providing care for this patient population. This may be a contributing factor to the role they feel family physicians should play in supporting these patients. Family physicians should be included in the transition process if patients have access to primary care. Future educational initiatives for adult rheumatologists and trainees should address the unique psychosocial concerns faced by youth with chronic rheumatic disease.
To cite this abstract in AMA style:
Prasad M, Batthish M, BEATTIE K, Berard R. Adult Rheumatologists’ Knowledge, Comfort Level, and Perceived Barriers in Supporting Newly Transitioned Youth with Chronic Rheumatic Diseases in Canada [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/adult-rheumatologists-knowledge-comfort-level-and-perceived-barriers-in-supporting-newly-transitioned-youth-with-chronic-rheumatic-diseases-in-canada/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/adult-rheumatologists-knowledge-comfort-level-and-perceived-barriers-in-supporting-newly-transitioned-youth-with-chronic-rheumatic-diseases-in-canada/