Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: A complex interaction between biologic factors and social determinants of health (SDoH) drives disparities in lupus (or SLE) outcomes in the US. A recent meta-analysis highlighted disparities in clinical outcomes for individuals with adverse SDoH. Yet, key SDoH that drive poor patient-reported outcomes (PROs)–patient’s self-evaluation of their health due to chronic disease, are not fully elucidated. Recently, a study using the California Lupus cohort highlighted that economic insecurities (i.e., food, housing, transportation, financial insecurity), not conventional SDoH (i.e., employment, insurance), were associated with poor PROs. Given geographical variations in lupus outcomes, we used our Wisconsin Lupus Cohort to: 1) identify key adverse SDoH, including economic insecurities, and SLE factors that associated with poor PROs in our cohort; 2) longitudinally examine the impact of addressing economic insecurities on PROs.
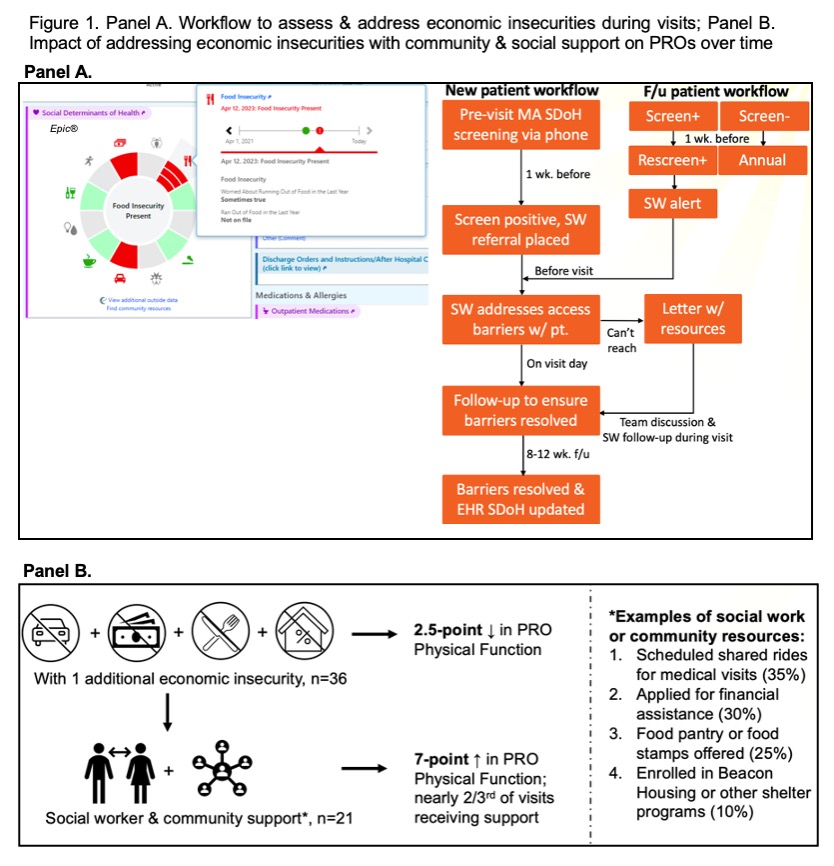
Methods: Our Wisconsin Lupus Cohort included adult patients with SLE recruited between 2020-24. Economic insecurities, including food, housing, transportation, and financial, were assessed by a medical assistant using screening questionnaires in the EHR (Fig. 1A). Economic insecurities were then addressed by a social worker (0.1 FTE) (Fig. 1A). Conventional SDoH, including area deprivation index (ADI), insurance, unemployment, high-risk behaviors, loneliness, were assessed. Patient-reported Physical, Mental, and Social Function T scores were derived from the PROMIS global health short form completed during visits. Associations between economic insecurities and PRO were assessed by multivariable linear regression models adjusting for demographics, SLE disease activity index (SLEDAI), SLE damage index (SDI), medicines, hydroxychloroquine (HCQ) levels, SLE duration, and conventional SDoH. A paired t-test longitudinally compared PRO before and after economic insecurities were addressed per workflow (Fig. 1A).
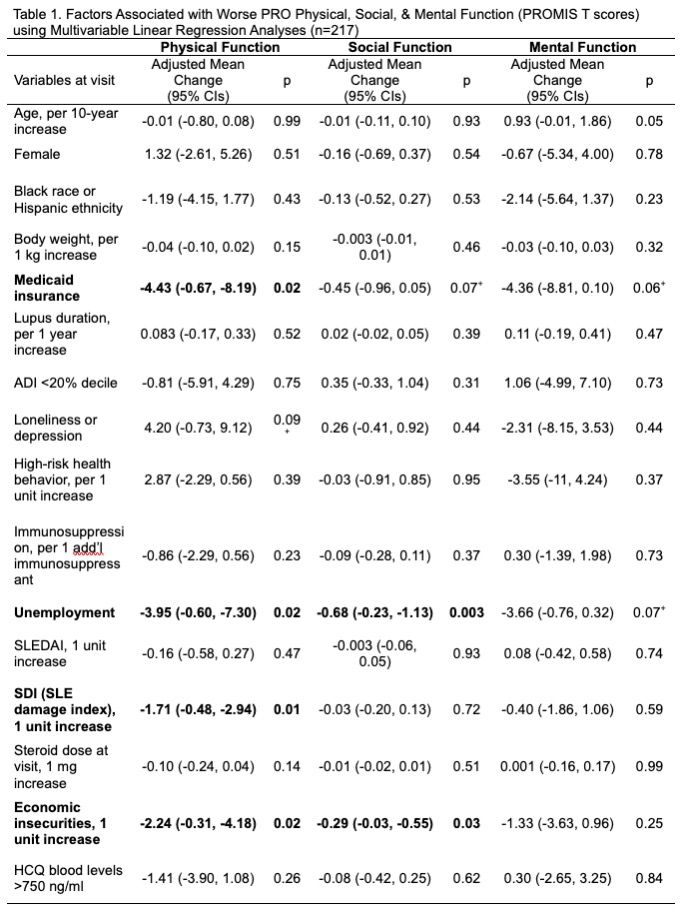
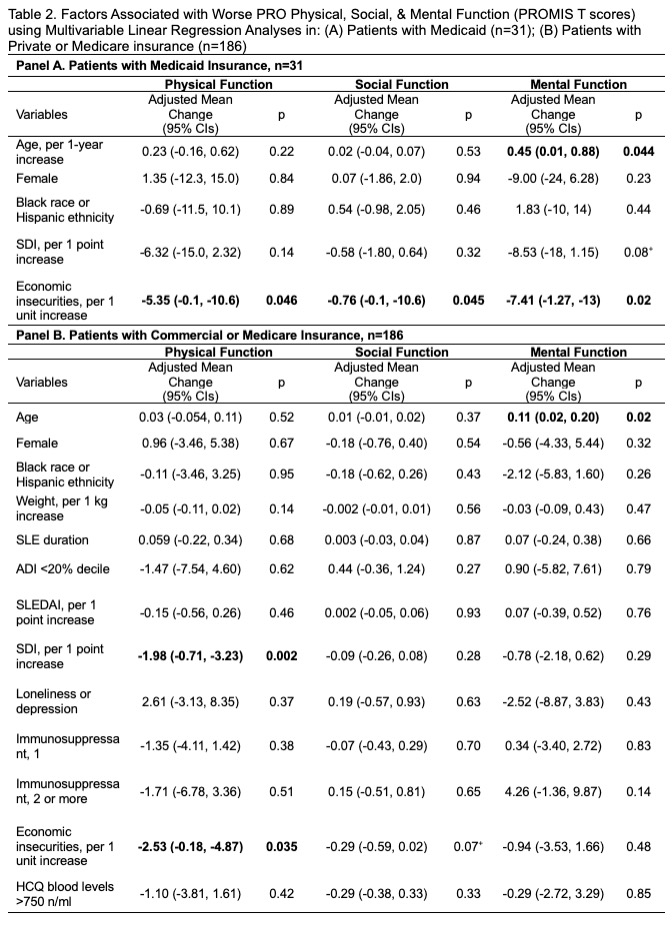
Results: Among 217 participants, mean age was 47±17 years, 90% were women, 27% were of Black race or Hispanic ethnicity, and 18% (n=36) had ≥1 economic insecurities. Multivariable analyses revealed that individuals with more economic insecurities had worse PRO vs. those without (Table 1). Every 1-unit increase in economic insecurities was associated with a 2.5-point decrease in Physical Function (p=0.02), a 0.33-point decrease in Social Function (p=0.02), a 2-point decrease in Mental Function (p=0.09). Conventional SDoH (unemployment, Medicaid) and SDI were also associated with worse PROs (Table 1). In two subgroups: 1) Medicaid insurance (n=31); 2) Private or Medicare insurance (n=186), economic insecurities remained strongly associated with worse PRO Physical, Mental, & Social Function (Table 2A-B).
Among 36 patients with ≥1 economic insecurities, 21 completed a follow-up visit within 6 mos. Economic insecurities were addressed in 58% of patients with a social worker’s support, and their Physical Function improved by 7 points (95% CIs 0.43-13, p-value=0.039; Fig. 1B).
Conclusion: Economic insecurities are associated with worse PROs which can be addressed with social work support and could improve outcomes and reduce disparities in SLE.
To cite this abstract in AMA style:
Garg S, Patel J, Ingersoll M, Gomez S, Weber A, Panzer S, Ferguson S, Singh T, Bartels C. Addressing Economic Insecurities Could Improve Patient-Reported Outcomes in Lupus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/addressing-economic-insecurities-could-improve-patient-reported-outcomes-in-lupus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/addressing-economic-insecurities-could-improve-patient-reported-outcomes-in-lupus/