Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Autoimmune myositis consists of a group of diseases with heterogeneous muscular and systemic manifestations. Prognosis also varies widely across the spectrum. Thus, myositis subgroups are being identified to facilitate personalized care. Systemic sclerosis (SSc) is a disease characterized by vasculopathy, autoimmunity, inflammation and fibrosis affecting multiple organs including muscle. The association of myositis and SSc is referred to as “scleromyositis”. Classification criteria for both myositis and SSc have been endorsed by ACR/EULAR but their performance for scleromyositis is unknown.
Methods: Patients with scleromyositis were identified in two centers. Diagnosis of scleromyositis was based on the co-existence of myositis and features of SSc according to expert opinion. Patients were systematically assessed for the presence or absence of items in the 2017 ACR/EULAR criteria for myositis and 2013 ACR/EULAR criteria for SSc at last follow-up. Additional organ involvement and auto-antibodies associated with myositis and SSc were also systematically recorded.
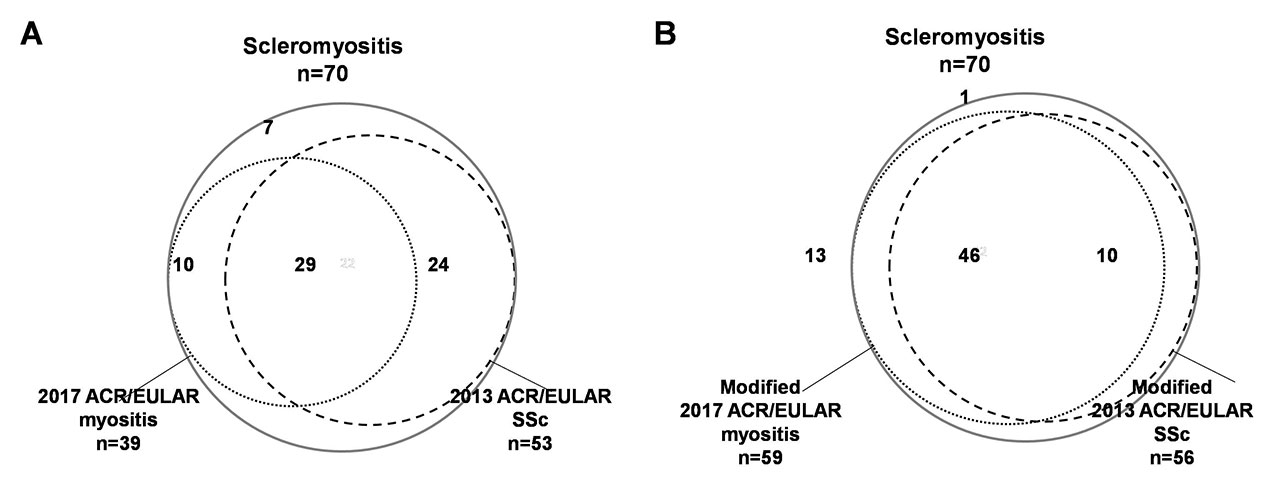
Results: Seventy (70) patients with scleromyositis (sex ratio F/M 3.7) were included. Age at myositis onset was 51.5 ± 15.8 years. Only 39 (56%) patients fulfilled the 2017 ACR/EULAR criteria for myositis (21 definite, 14 probable, 4 possible) and 53 patients (76%) fulfilled the 2013 ACR/EULAR criteria for SSc (Figure 1). Of these, only 29 (41%) fulfilled both sets of criteria. Seven (10%) patients fulfilled neither set of criteria (Figure 1a). The ACR/EULAR criteria that were most frequently lacking for myositis were anti-Jo1 antibodies (n=70, 100%) and dermatomyositis rash (Gottron sign, Gottron papule and/or heliotrope rash n=61, 87%). The criteria that were most frequently lacking for SSc were pulmonary arterial hypertension (n=68, 97%) and “classical” SSc auto-antibodies (anti-Scl70, -centromere, -RNA polymerase III, n= 63, 90%). The 7 patients fulfilling neither ACR/EULAR criteria for myositis nor SSc all had increased creatinine kinase and Raynaud’s phenomenon, but the frequency of the other items in the criteria were all < 50%. Four of the 7 patients (56%) had well-known complications of SSc some of which are not included in the criteria: interstitial lung disease (n=3), calcinosis (n=1) and/or renal crisis (n=1). All 7 patients had auto-antibodies associated with scleromyositis that are also not included in ACR/EULAR criteria: anti-Ku (n=3), anti-SMN1 (n=2), anti-PM/Scl (n=1), anti-U1RNP (n=1) and/or anti-RuvBL1/2 (n=1), When ACR/EULAR criteria for myositis and SSc were modified to take into account these additional clinical features and auto-antibodies, the rate of patients who fulfilled myositis and SSc criteria increased from 41% to 66% (Figure 1b).
Conclusion: In our cohort, ACR/EULAR criteria for myositis and SSc alone and together had low sensitivity for scleromyositis. Additional clinical features and serologies could lead to improved sensitivity. Studies of scleromyositis will require careful consideration of inclusion criteria to ensure that the full spectrum of this important subset is included.
To cite this abstract in AMA style:
Meyer A, Leclair V, Landon-Cardinal O, Ellezam B, D'Aoust J, Giannini M, Geny B, Arnaud L, Gottenberg J, Sibilia J, Satoh M, Fritzler M, Troyanov Y, Hudson M. ACR/EULAR Criteria for Myositis and Systemic Sclerosis Lack Sensitivity for Scleromyositis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/acr-eular-criteria-for-myositis-and-systemic-sclerosis-lack-sensitivity-for-scleromyositis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/acr-eular-criteria-for-myositis-and-systemic-sclerosis-lack-sensitivity-for-scleromyositis/