Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Session Type: Poster Breakout Session
Session Time: 5:10PM-5:40PM
Background/Purpose: The pattern of arterial involvement and disease severity varies in those affected with cTA. Distinct imaging patterns that have some congruence with clinical phenotype may guide prognosis and treatment decisions. We aim to identify radiographic ‘classification” patterns in cTA using data driven, unsupervised machine learning and to determine if they associate with distinct clinical phenotypes and disease course.
Methods: We analyzed data from ARChiVe (A Registry for Childhood Vasculitis) patients who met either the American College of Rheumatology (ACR) criteria or the European League against Rheumatism (EULAR)/Pediatric Rheumatology International Trials Organization (PRINTO)/Pediatric Rheumatology European Society (PRES) classification criteria for cTA. Multilayer non-negative matrix factorization (NMF) was conducted to identify patterns of co-involved vessel segments at presentation. NMF dimensionally reduces a larger number of variables to a parts-based representation comprising a smaller number of summary variables or “factors,” analogous to parts of faces. We assigned patients to groups by their highest-scoring pattern. We determined associations between each group and demographics, clinical symptoms, treatment and outcome by linear regression on ranks and Cox proportional hazards modelling.
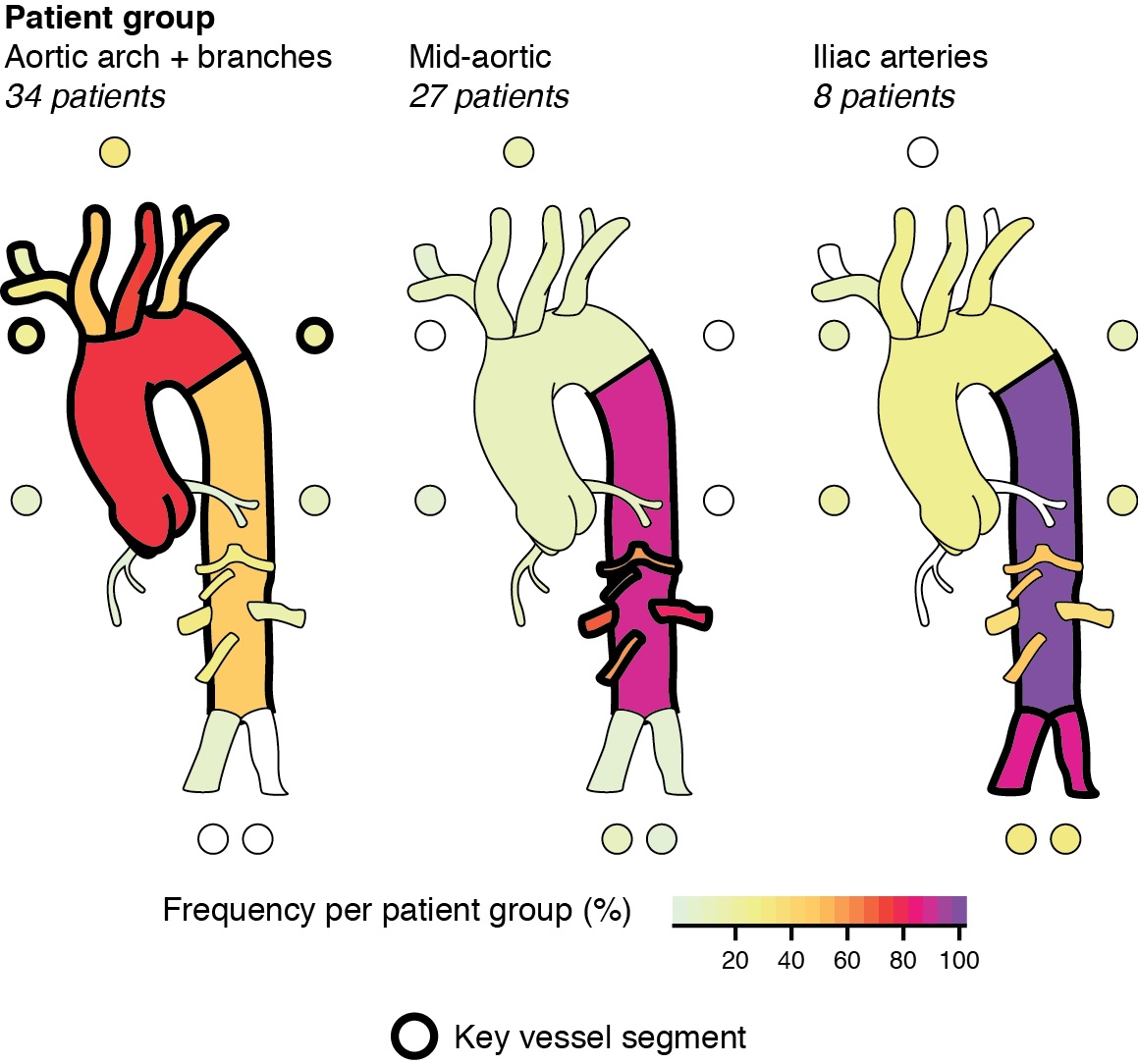
Results: A total of 70 patients were included. NMF identified three patterns of vessel involvement leading thus discriminating three groups of patients. Group one (n=34, 48.6%) had predominant involvement of the aortic arch and its branches;they are more likely to be female, have central nervous system symptoms, and be treated with anti-platelet agents. Group two (n=27, 38.6%), distinguished by mid-aortic vessel disease, have more renal involvement and are more likely to be on an anti-hypertensive drug. At 6 months after diagnosis, they continue to have cardiovascular and renal symptoms, abnormal platelet count, and higher pediatric vasculitis activity score (PVAS) and physician global assessment scores. At 12 months after diagnosis, they have more constitutional symptoms and abnormal inflammation markers (white cell count, platelet count and CRP). Group three (n=8, 11.4%) distinguished by iliac artery disease. They report more mucous membrane symptoms and limb claudication, have abnormal platelet counts and higher PVAS scores at baseline. A higher proportion of this group have abnormal hemoglobin at 12 months after diagnosis. Pediatric vascular damage index (PVDI) is higher in this group at 6 and 12 months after diagnosis. There was no significant difference in the medications administered between the 3 groups.
Conclusion: Established analytical framework identified 3 distinct groupings of involved vessels in cTA that associate with characteristic clinical presentations and disease course.. Children with mid-aortic disease have ongoing disease activity while children with iliac artery disease have higher disease damage on follow-up suggesting that both groups require more intensive therapy.
To cite this abstract in AMA style:
Go E, Eng S, Cabral D, Yeung R. A Preliminary Data-driven Anatomic Classification for Childhood Takayasu Arteritis (cTA) [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/a-preliminary-data-driven-anatomic-classification-for-childhood-takayasu-arteritis-cta/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-preliminary-data-driven-anatomic-classification-for-childhood-takayasu-arteritis-cta/