Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The ACGME’s core competencies for pediatric residency training include medical knowledge, patient care, and interpersonal communication skills. At our institution, residents only spend two weeks or fewer rotating through pediatric rheumatology. A needs assessment among pediatric rheumatology attendings identified key rare disease states that are unlikely to be clinically encountered by learners during this short time. High-fidelity simulation is an effective tool in pediatric medical education1. We designed a simulation module to expose pediatric learners to two such rheumatologic diseases with clinically distinct, recognizable disease presentation patterns. Learning objectives included: 1) Recognize juvenile dermatomyositis (JDM); 2) Recognize macrophage activation syndrome (MAS); 3) Successfully consult a subspecialist. This intervention was developed to increase learner exposure to rare rheumatologic diseases during limited time on the pediatric rheumatology rotation.
Methods: We collaborated with our institution’s pediatric simulation center to create these educational modules focused on pediatric rheumatology. After several months of development, we piloted the modules with final- year medical students and pediatric residents during their clinical rotations.. Local IRB approval was obtained. Participants completed the simulation module as a group and underwent botha pre- and post-simulation questionnaire assessing knowledge pertaining to subject material covered in the module. A post-simulation debriefing simulation in accordance with the standard simulation teaching modality. Descriptive statistics and one-sided t-tests assuming equal variance were used for data analysis.
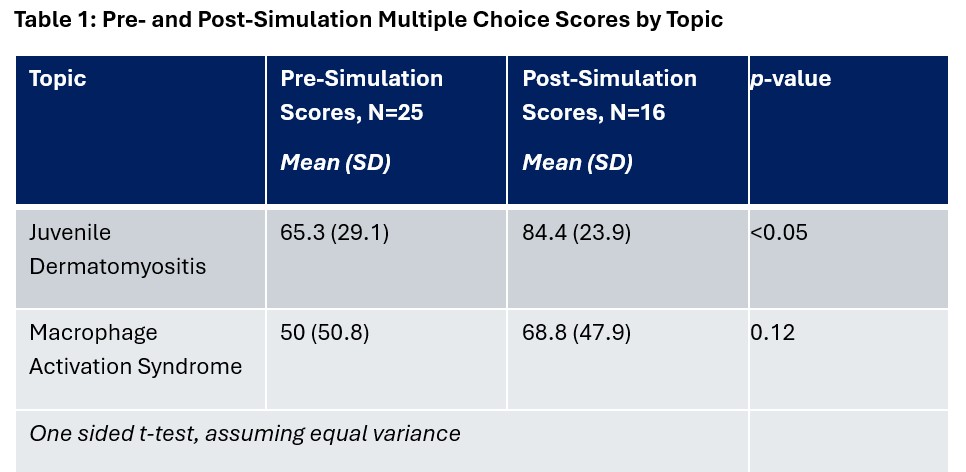
Results: A multiple choice questionnaire was distributed as a pre- and post-module assessment of learner knowledge regarding MAS and JDM. Learner confidence in diagnostic recognition and in subspecialist consultation was measured using a 5 point Likert scale. Mean percent correct responses increased from 65.3 (SD 29.1) to 84.4 (SD 23.9) for JDM and from 50 (SD 50.8) to 68.8 (SD 47.9) for MAS, respectively. Confidence in diagnostic suspicion of JDM increased from mean of 2.78 to 3.8 and for MAS increased from 2.88 to 3.9. Confidence in subspecialist consultation increased from 3.45 to 4.3. 100% of learners surveyed reported that the simulation module was a helpful learning activity for the rotation.
Conclusion: This pilot module of high-fidelity simulation for pediatric learners demonstrates knowledge acquisition and increased learner confidence in important core competencies. The long-term goal of this work is to design additional sessions into a modular curriculum for utilization by any training program with access to a simulation center. High-fidelity simulation in pediatric rheumatology is a promising educational method that has the potential to increase access to pediatric learning during medical school and residency training, which could lead to significant improvements in disease recognition and prompt referral in the setting of pediatric rheumatology workforce challenges and large numbers of unnecessary referrals2,3.
To cite this abstract in AMA style:
Bridges J, Timmerman L, Rockwell N. A Pilot High-Fidelity Simulation for Pediatric Rheumatology Learners [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/a-pilot-high-fidelity-simulation-for-pediatric-rheumatology-learners/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-pilot-high-fidelity-simulation-for-pediatric-rheumatology-learners/

.jpg)