Session Information
Date: Sunday, November 7, 2021
Title: Epidemiology & Public Health Poster II: Inflammatory Arthritis – RA, SpA, & Gout (0560–0593)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatoid arthritis (RA) is recognized to increase the risk of premature death. The impact of RA on survival varies across causes of death, though few studies have precisely estimated mortality risk for specific causes. While all-cause mortality appears to be improving, perhaps due to advances in care, it remains unclear how these advances have impacted cause-specific mortality, particularly relative to the non-RA population. We examined risk and temporal trends in all-cause and cause-specific mortality in RA in the Veterans Health Administration (VHA), the largest integrated healthcare system in the U.S.
Methods: We conducted a retrospective, matched cohort study in the VHA from 1/1/2000-12/31/2017. RA patients (≥2 ICD codes for RA, rheumatologist diagnosis, and a positive autoantibody or DMARD fill) were matched up to 1:10 on age, sex, and year of VHA enrollment to non-RA patients. RA was considered incident if they received care in the VHA for ≥365 days without a RA diagnostic code or DMARD fill. Patients were followed from fulfillment of the RA algorithm (corresponding calendar date for non-RA) until death or end of study period. Vital status and cause of death were obtained from the National Death Index. Baseline covariates were obtained from national VHA databases and included demographics, smoking status, BMI, Rheumatic Disease Comorbidity Index, and health care utilization. Cox regression was used to examine the association of RA with all-cause and cause-specific mortality.
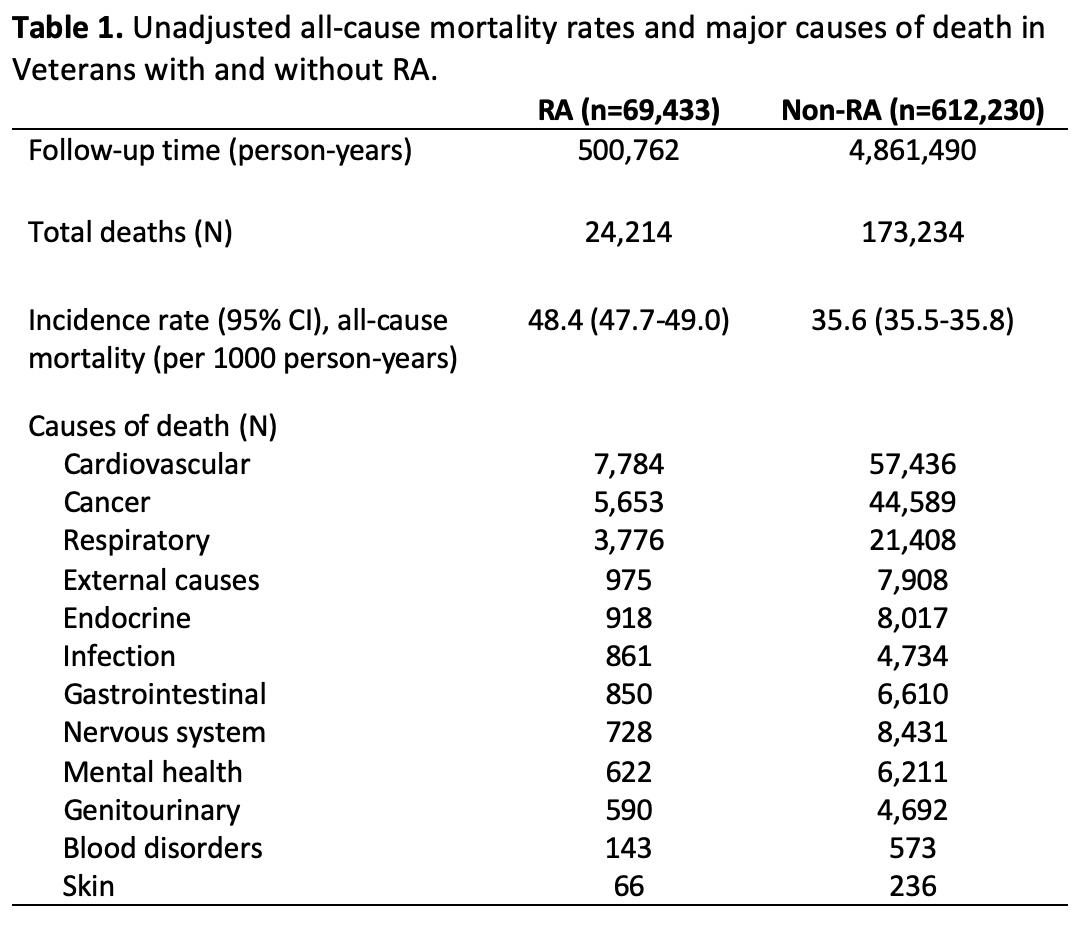
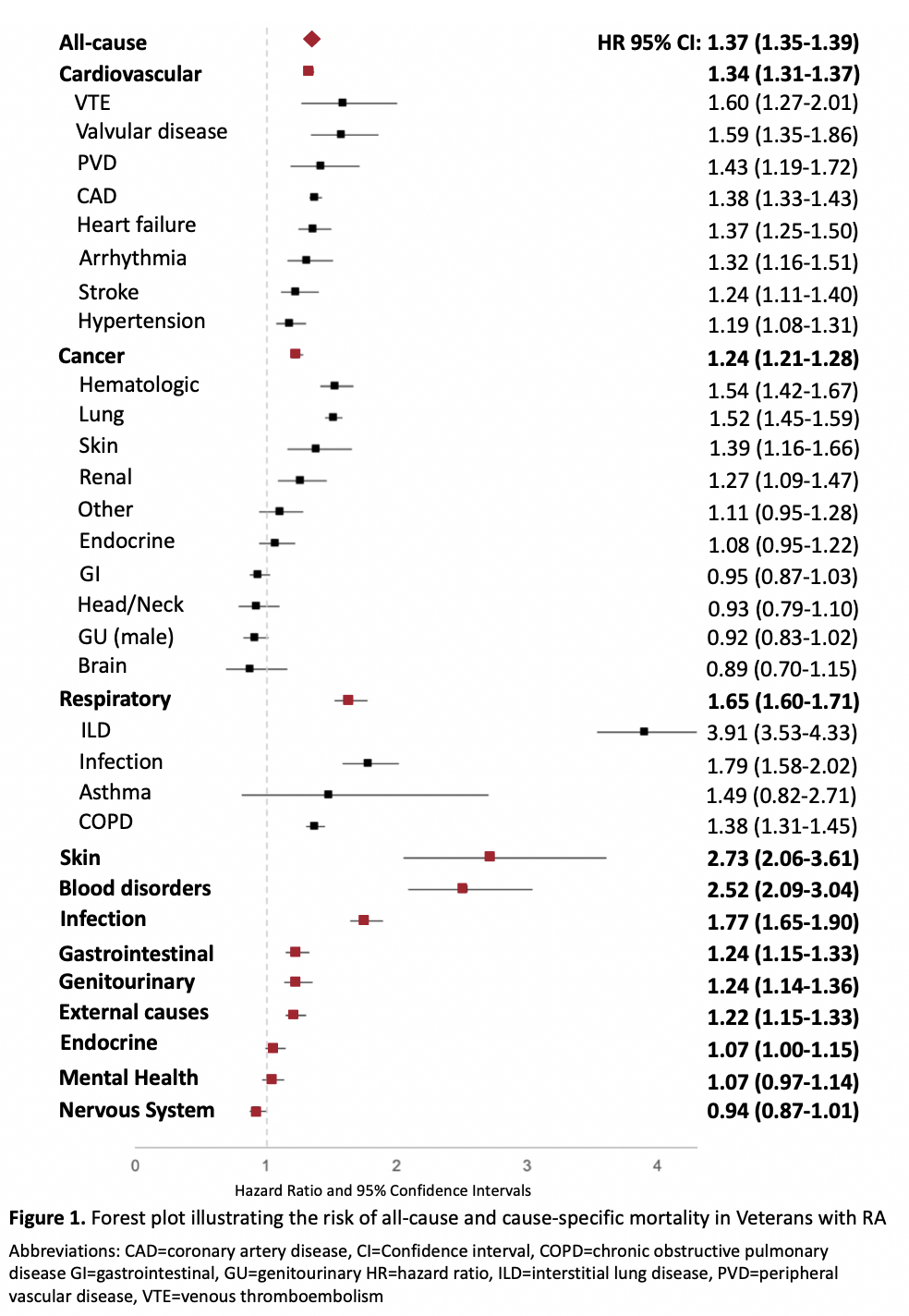
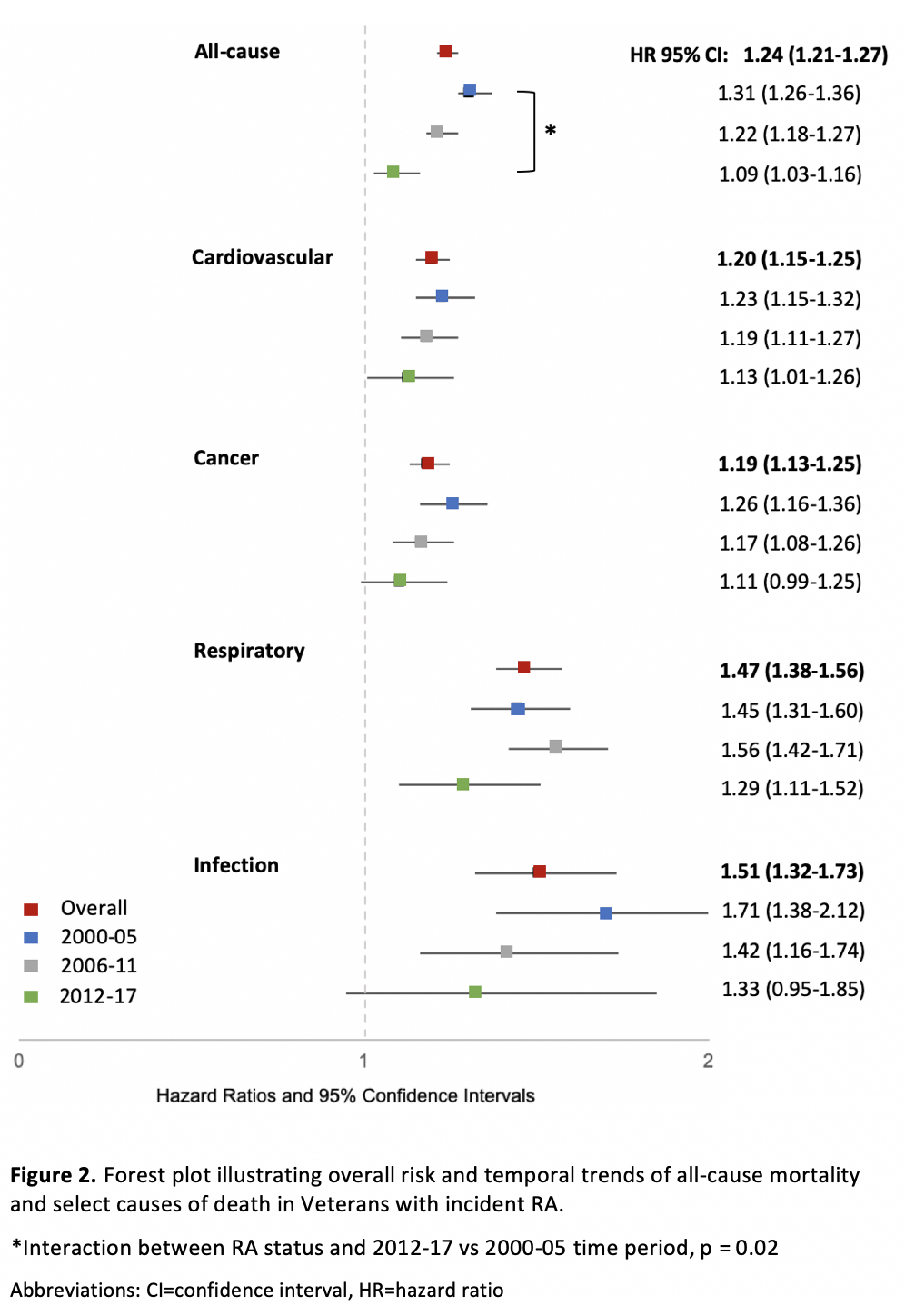
Results: We matched 69,433 RA patients (n=48,828 incident RA) to 612,230 non-RA patients. RA patients in this study were predominantly male (88.0%), had a mean age of 63 years, and were more frequently current smokers with greater comorbidity compared to non-RA. Crude incidence rates and causes of death are detailed in Table 1. After multivariable adjustment, RA patients were at increased risk of all-cause (HR 1.37 [95% CI 1.35-1.39]), cardiovascular (HR 1.34 [1.31-1.37]), cancer (HR 1.24 [1.21-1.28]), respiratory (HR 1.65 [1.60-1.71]), and infection-related mortality (HR 1.77, 1.65-1.90), as well as other less frequent causes (Figure 1). Within these major causes of death, interstitial lung disease (ILD)-related deaths were most closely associated with RA (HR 3.91 [3.53-4.33]). Results were similar in the incident RA cohort. In the incident cohort, all-cause mortality risk related to RA was significantly lower during 2012-2017 compared to 2000-2005 (Figure 2), but still higher compared to non-RA. RA-associated risk for cardiovascular, cancer, respiratory, and infectious mortality were also numerically lowest in 2012-2017 but remained higher compared to non-RA.
Conclusion: In a national study of US veterans with and without RA from 2000-2017, we estimated a 37% increased risk of all-cause mortality in RA. Excess mortality was driven by cardiovascular, cancer, and respiratory causes, particularly ILD which was the most overrepresented cause of death in RA. Though our findings provide further support that RA-related mortality risk is improving over time, a mortality gap remains for all-cause and cause-specific mortality in RA suggesting continued efforts are needed to improve longevity.
To cite this abstract in AMA style:
Johnson T, Yang Y, Roul P, Sauer B, Baker J, Mikuls T, England B. A Narrowed, but Persistent Mortality Gap: A National, Matched Cohort Study in U.S. Veterans with Rheumatoid Arthritis from 2000-2017 [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/a-narrowed-but-persistent-mortality-gap-a-national-matched-cohort-study-in-u-s-veterans-with-rheumatoid-arthritis-from-2000-2017/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-narrowed-but-persistent-mortality-gap-a-national-matched-cohort-study-in-u-s-veterans-with-rheumatoid-arthritis-from-2000-2017/