Session Information
Date: Monday, November 9, 2015
Title: Miscellaneous Rheumatic and Inflammatory Diseases Poster Session II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
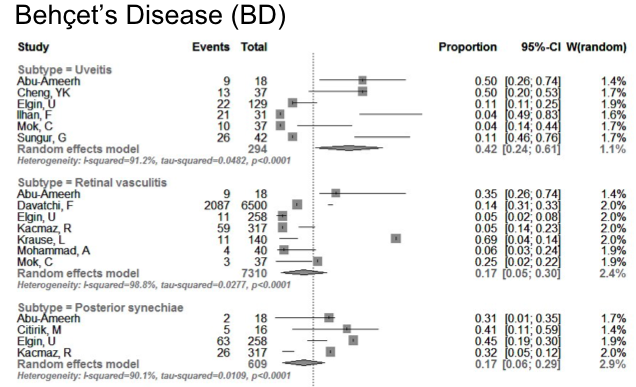
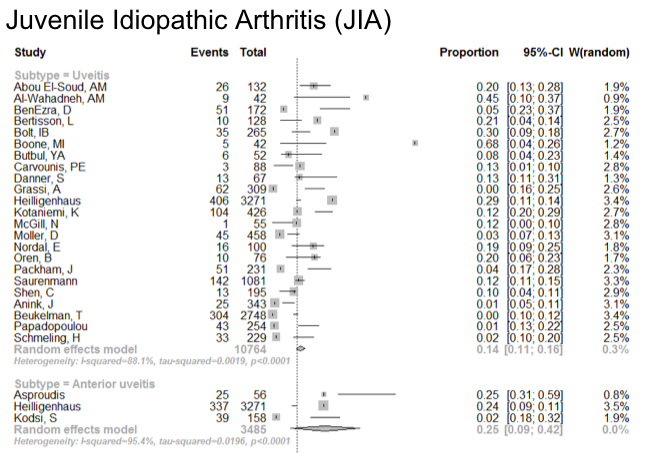
Background/Purpose: Many inflammatory rheumatic diseases (IRD) are
associated with ocular involvement. The prevalence of these complications is
not fully known. This meta-analysis was performed to systematically
investigate the prevalence and type of ocular involvement in IRD.
Methods: Medline, Web of Science and Cochrane databases were
searched to July 2014, to identify publications related to IRD and associated
ocular conditions. Disease terms included; juvenile arthritis (JIA), rheumatoid
arthritis (RA), connective tissue disease, spondyloarthropathy (SpA), ankylosing
spondylitis (AS) and Behcet’s disease. For eye involvement terms were;
conjunctivitis, keratoconjunctivitis sicca, xeropthalmia, uveitis, eye
hemorrhage, optic neuritis, papilledema, orbital disease, retinal artery/vein
occlusion, macular edema, retinitis, chorioretinitis, scleritis,
iridocyclitits, choroid hemorrhage, blindness and amaurosis fugax. Data
regarding the rates of ocular complications were analyzed with a random effects
model.
Results: 7124 studies were found with 263
for full review. There were 13 AS studies, 30 Behcet’s disease (BD), 31 JIA, 12
PsA, 11 RA and 165 others. Pooled prevalence for commonly reported ocular
manifestation were uveitis rates of: 22% (95% CI: 16-24%) in AS, Behcet’s 55%
(41-68%), JIA [oligoarthritis 36% (20-51%), polyarticular 13% (8-19%) systemic
onset 3% (0-7%)], pediatric Behcet’s 33% (0-74%), and PsA 15% (5-24%) for
anterior uveitis and 0.2% for posterior uveitis. In RA, keratoconjunctivitis
sicca occurred in 16% (8-25%), sicca symptoms in 31% (21-42%), marginal
ulcerative keratitis in 1-3%, episcleritis in 1-2% and retinal vasculitis in
0.2%. In SLE 29% of patients had dry eyes. There may have been publication bias
(over reporting due to selection bias of cohorts enriched for ocular complications
such as patients from university clinics where complications could be higher,
and several estimates had herterogeneity. Data were lacking on confounding
variables (such as screening and treatment). Figure
shows some uveitis rates.
Conclusion:
Extra-articular manifestations of inflammatory rheumatic diseases frequently
complicate the ocular health of afflicted individuals. Although the rates vary,
an awareness of potential complications can aid in early identification and
treatment of these rheumatic complications. Rates of ocular involvement may not
be changing over time and therefore need to be recognized and treated
appropriately.
 .
.
To cite this abstract in AMA style:
Hayworth J, Pope JE. A Meta-Analysis of the Prevalence of the Ocular Manifestations in All Inflammatory Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/a-meta-analysis-of-the-prevalence-of-the-ocular-manifestations-in-all-inflammatory-rheumatic-diseases/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-meta-analysis-of-the-prevalence-of-the-ocular-manifestations-in-all-inflammatory-rheumatic-diseases/
