Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: COVID-19 infection frequently leads to a cytokine storm, which has successfully been treated with some immunomodulating therapies according to observational studies. Interestingly, treatments investigated for the management of COVID-19 significantly overlap with those used in rheumatoid arthritis (RA). We aimed to investigate the prevalence and predictors of COVID-19 infection, severe infection requiring emergency department (ED) visits, hospitalization, intensive care unit (ICU) admission, intubation, and mortality in RA.
Methods: This was a cross-sectional analysis by linking the RA patients from the Ontario Best Practices Research Initiative (OBRI) to Institute for Clinical Evaluative Sciences (ICES) administrative data containing all health care records for Ontarians to explore the COVID-19 infection, hospital/intensive care unit (ICU) admissions and mortality due to COVID-19 (between Jan 1 2020 – Mar 31 2022). Primary outcome COVID-19 infection event was defined if patient had any positive COVID-19 test or diagnosis code ‘080’ in Ontario health insurance program (OHIP) during study period. We also looked at admission to hospital, ICU, required intubation, and death following COVID-19 infection. Characteristics of patients were compared between patients with and without covid-19 infection within 2 years before and 3 months after COVID-19 pandemic (15 March 2020). We also looked at the association of patient’s characteristics and risk of COVID-19 infection using multivariable logistic regression models.
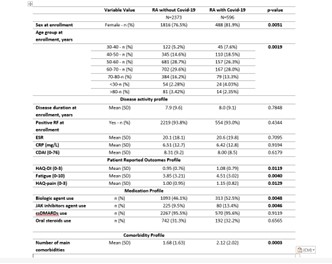
Results: A total of 2969 patients were included. Among these, 596 (20.1%) were reported as having had COVID-19 infection. Females were significantly more likely to have infection (Covid-19 group: 81.9% vs. non-covid-19: 76.5%) (Table 1). There was no difference in disease duration between two groups. Patient reported outcome (e.g. HAQ-DI, fatigue, and pain) and number of comorbidities was significantly higher in patients with COVID-19 infection. Patients with COVID-19 were more likely to use biologic agents (52.5% vs. 46.1%) and JAK inhibitors (13.4% vs. 9.5%).
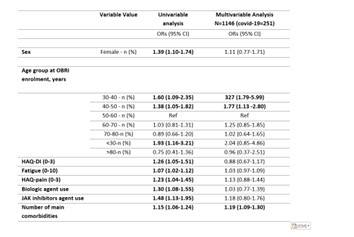
There was a significant positive association between age younger than 50 years (adj ORs: 3.27; 95%CI: 1.79-5.99 and 1.77; 95%CI: 1.13-2.80 for 30-40 and 40-50 age group, respectively) and higher number of comorbidities (adj ORs: 1.19; 95%CI: 1.09-1.30) and risk of COVID-19 infection in multivariable analysis (Table 2). Out of 596 patients with covid-19 infection, 108 (18.1%) had a record of ED visit or hospitalization. Among 108 ED visits or hospitalization, 13 (12.0%) admitted to the ICU, 11 (10.2%) admitted to ICU and had intubation, one (0.93%) had only intubation, and 28 (25.9%) died during follow-up.
Conclusion: In this study we found that COVID-19 infection was higher in female patients, younger than 50 years old, and those with higher number of comorbidities.
To cite this abstract in AMA style:
Movahedi M, Hepworth E, Cesta A, Li X, Bombardier C, Aydin S. A Cross-sectional Study on Predictors of COVID-19 Infection, Admission and Mortality and Effect of Immunomodulating Treatments in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/a-cross-sectional-study-on-predictors-of-covid-19-infection-admission-and-mortality-and-effect-of-immunomodulating-treatments-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-cross-sectional-study-on-predictors-of-covid-19-infection-admission-and-mortality-and-effect-of-immunomodulating-treatments-in-rheumatoid-arthritis/