Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: SLE is a systemic autoimmune disease that can present at different ages and with various multiorgan complications. In this study, we aimed to analyze the differences in characteristics in patients with older onset SLE (age of diagnosis >50) and younger onset SLE (age of diagnosis 49).
Methods: A retrospective cohort study was performed using TriNetX, a global federated health research network that provides access to electronic medical records across large health care organizations (HCOs). Data was used from 99 different HCOs. Adult patients (>18 years of age) were divided into two cohorts, older and younger onset SLE, based on age of SLE diagnosis (ICD-10: M32.9). 1:1 propensity score matching was performed using 58 different baseline patient characteristics, including demographics, comorbidities, medication usage, and serological profiles (Table 1 and Table 2). Kaplan-Meier survival analysis was performed to examine differences in mortality between both cohorts.
Results: 62,242 patients were included in the older onset SLE cohort and 85,011 patients were included in the younger onset SLE cohort before propensity score matching. After propensity score matching, 45,733 patients were included in the older onset SLE and younger onset SLE cohorts respectively. Univariate analysis before matching showed several significant differences in characteristics between both cohorts (Table 1 and Table 2). After propensity score matching, the frequency of thrombocytopenia was higher in the younger onset SLE group compared to the older onset SLE cohort (p < 0.001), otherwise the frequency of SLE related comorbidities was not significantly different (Table 1). Patients in the younger onset SLE cohort had a higher frequency of positive anti-dsDNA (p < 0.001), positive anti-RNP (p < 0.001), and low complement C3 and C4 (p < 0.001) (Table 2). There were no statistically significant differences in the frequencies of medications used (Table 2). Risk analysis showed that 4,658 (10.2%) of older onset SLE patients died and 1,896 (4.1%) of younger onset SLE patients died during the study period (7,000 days) (RR = 2.457, 95% CI 2.333, 2.587, p = < 0.001). Survival analysis revealed that the older onset SLE group had a markedly lower survival probability at the end of the observation period (51.79%) compared to those diagnosed before age 49 (82.38%). The difference in survival between groups was statistically significant (log-rank test χ² = 1515.153, p < 0.001). Cox proportional hazards modeling showed that older onset SLE was associated with a significantly increased risk of mortality (hazard ratio: 2.77; 95% CI: 2.63–2.92). The assumption of proportional hazards was met (χ² = 1.466, p = 0.226), supporting the validity of the model (Figure 1).
Conclusion: This retrospective cohort study suggests that younger onset SLE patients are more likely to develop thrombocytopenia, otherwise have no significant difference in the examined comorbidities. Patients with younger onset SLE are also more likely to have positive anti-dsDNA, positive anti-RNP, and hypocomplementemia. Medications used between younger and onset SLE patients are not significantly different. Patients with older onset SLE have a significantly increased risk of mortality.
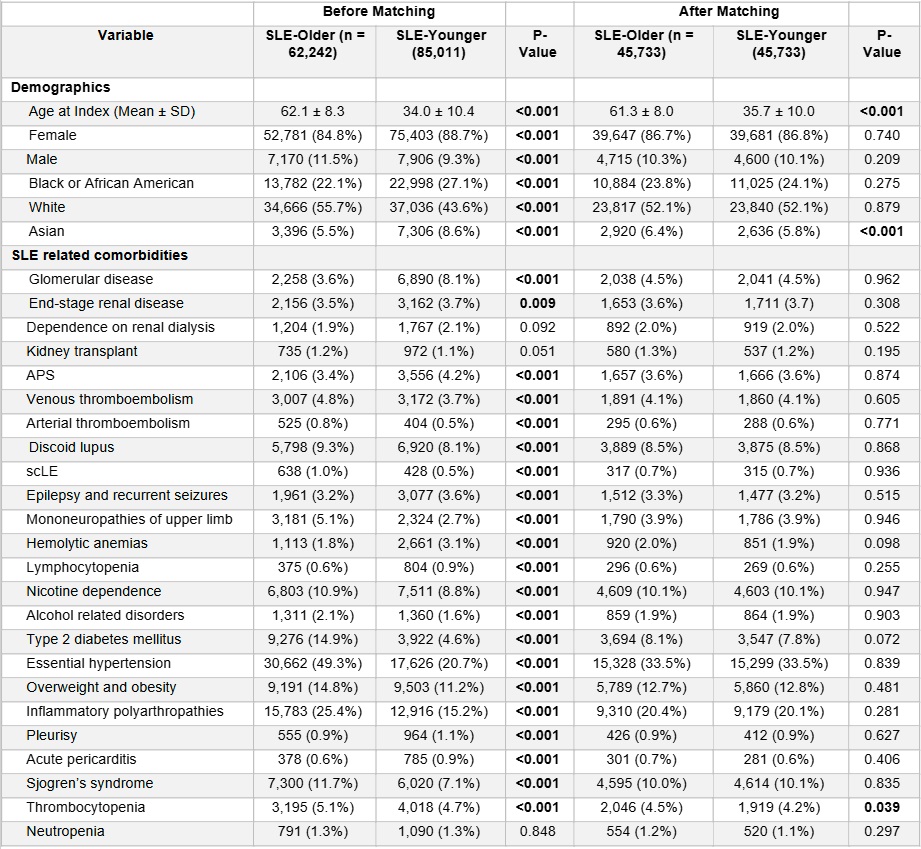 Table 1. Baseline Characteristics of Older Onset SLE Patients vs. Younger Onset SLE Patients
Table 1. Baseline Characteristics of Older Onset SLE Patients vs. Younger Onset SLE Patients
.jpg) Table 2. Serological Profiles and Medications Used in Older Onset SLE patients vs. Younger Onset SLE Patients
Table 2. Serological Profiles and Medications Used in Older Onset SLE patients vs. Younger Onset SLE Patients
.jpg) Figure 1. Kaplan-Meier Survival Analysis of Mortality in Older Onset SLE Patients vs. Younger Onset SLE Patients
Figure 1. Kaplan-Meier Survival Analysis of Mortality in Older Onset SLE Patients vs. Younger Onset SLE Patients
To cite this abstract in AMA style:
Guan C, Heydari-Kamjani M, Pfeil K, Harper E, Frumker L, Gump M, Pamuk O. A Comparison of Patients with Older Onset vs. Younger Onset SLE: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/a-comparison-of-patients-with-older-onset-vs-younger-onset-sle-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-comparison-of-patients-with-older-onset-vs-younger-onset-sle-a-retrospective-cohort-study/
