Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatoid arthritis (RA) guidelines suggest management according to “treat-to-target,” with escalation of treatment in patients with moderate/high (M/H) DAS28 (disease activity score 28) or CDAI (clinical disease activity index) according to shared decisions toward low activity/remission (R/L). It is recognized that elevated RA clinical core data set measures and indices may be seen in the absence of inflammatory activity in RA patients with comorbid joint damage and/or fibromyalgia. A multidimensional health assessment questionnaire (MDHAQ) includes queries to screen for fatigue, back pain, neck pain, headache, problems with sleep or thinking, and indices to screen for anxiety, depression and fibromyalgia. Analyses were performed of RA patients with 0 or 1 swollen and tender joint counts (SJC & TJC), who met criteria for remission according to these measures, but who were classified as M/H on DAS28-ESR (disease activity score 28–erythrocyte sedimentation rate) , CDAI (clinical disease activity index), or RAPID3 (routine assessment of patient index data) and would be regarded as candidates for escalation of therapy, to identify comorbidities found on the MDHAQ which may explain the elevated index scores.
Methods: Unselected patients with RA seen in routine care completed an MDHAQ prior to seeing the rheumatologist, who performed a standard 28 joint count. DAS28–ESR, CDAI, and RAPID3 were computed, and patients were classified as L/R or M/H. The proportion of patients who were identified as having each of 9 generally non-inflammatory comorbidities on the MDHAQ and any of 9 was computed for each index, recognizing that these comorbidities may reflect inflammation in certain patients.
Results: In 173 patients with RA seen in 2021, SJC and TJC 0 or 1 was found in 73 (42%), of whom 7%, 34%, and 58% were classified as M/H according to DAS28-ESR, CDAI, and RAPID3, respectively. Among these patients, positive MDHAQ screening was seen in 29-33% for anxiety , 26-33% for depression, 17-38% for fibromyalgia, 67-81% for fatigue >3/10, 48-67% for back pain, 50-57% for neck pain, 0-21% for headache, 43-63% for problems with sleep and 0-33% for problems with thinking. One of the 9 comorbidities was seen in 86-96% of patients with SJC and TJC 0 or 1, who were classified as M/H (Table). In patients with SJC and TJC 0 or 1 who were classified as R/L, 47%-68% reported one of the 9 symptoms. The proportion reporting each symptom was higher in the M/H group for all 3 indices other than two symptoms reported by none of 7 patients with 0 or 1 SJC and TJC who were classified as DAS28–ESR M/H (Table).
Conclusion: In 173 patients with RA seen in 2021 who met SJC and TJC criteria for remission but were classified as DAS28-ESR, CDAI, or RAPID3, 86-96% reported one of 9 non-inflammatory comorbidities on the MDHAQ found on the MDHAQ. One limitation is that it is possible that one or more comorbidities identified as “non-inflammatory” may result from inflammation in certain patients. Nonetheless, the MDHAQ, which is completed by most patients in 5-10 minutes and is available in the February 2025 release of the Epic electronic medical record (EMR), can be helpful to interpret RA index scores for treat-to-target, description of outcomes, and general patient management.
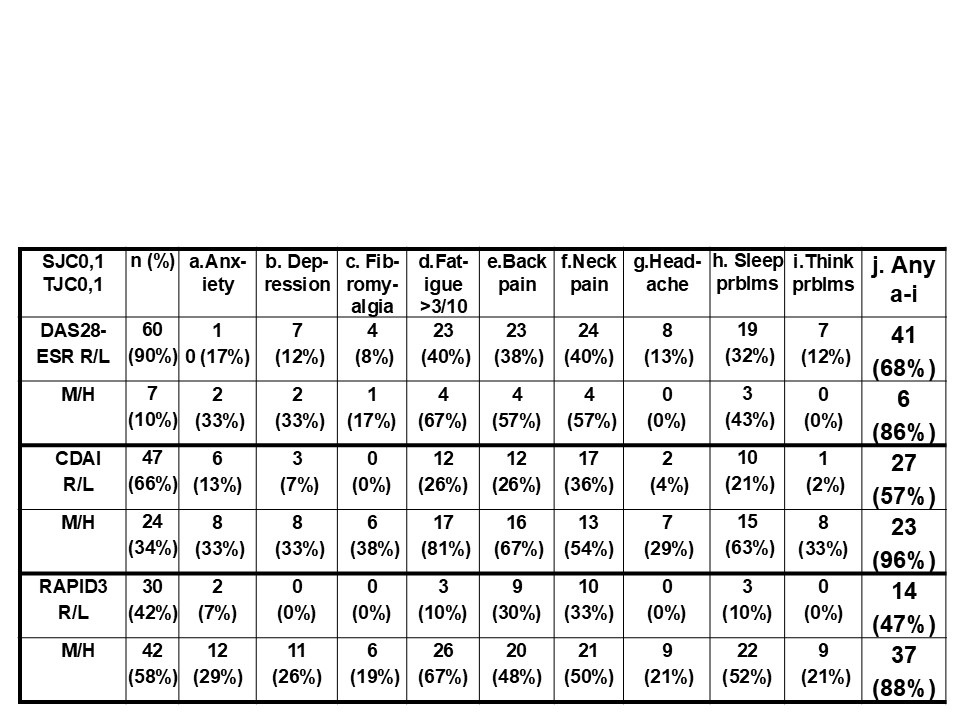 Proportion of Rheumatoid arthritis patients with 0 and 1 swollen (SJC) and tender (TJC) joints on a 28 joint count who reported positive responses for 9 comorbidities within the MDHAQ vs classification as DAS28–ESR, CDAI, or RAPID3 remission/low (R/L) or moderate/high (M/H)
Proportion of Rheumatoid arthritis patients with 0 and 1 swollen (SJC) and tender (TJC) joints on a 28 joint count who reported positive responses for 9 comorbidities within the MDHAQ vs classification as DAS28–ESR, CDAI, or RAPID3 remission/low (R/L) or moderate/high (M/H)
To cite this abstract in AMA style:
Pincus T, Schmukler J, Li T. 86-96% of rheumatoid arthritis (RA) patients with RA who have 0 or 1 swollen joint or tender joint but are classified as moderate/high on RA indices have 1-9 comorbidities recognized on a multidimensional health assessment questionnaire (MDHAQ) [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/86-96-of-rheumatoid-arthritis-ra-patients-with-ra-who-have-0-or-1-swollen-joint-or-tender-joint-but-are-classified-as-moderate-high-on-ra-indices-have-1-9-comorbidities-recognized-on-a-multidimensio/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/86-96-of-rheumatoid-arthritis-ra-patients-with-ra-who-have-0-or-1-swollen-joint-or-tender-joint-but-are-classified-as-moderate-high-on-ra-indices-have-1-9-comorbidities-recognized-on-a-multidimensio/
