Session Information
Date: Wednesday, October 29, 2025
Title: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders II (2699–2704)
Session Type: Abstract Session
Session Time: 12:00PM-12:15PM
Background/Purpose: The prevalence of ocular involvement (OI) in patients with relapsing polychondritis (RP) has not been well defined. This study aimed to describe ocular manifestations, other clinical features, and use of immunosuppressive agents (IS), in patients with RP with and without OI.
Methods: The study included adult patients with physician-diagnosed RP enrolled in a multicenter prospective observational cohort [University of Pennsylvania (Penn) and the National Institutes of Health (NIH)]. Data on demographics, clinical presentations, including OI, and use of IS [glucocorticoids (GC), non-biologic, and biologic IS] were collected. Means with standard deviation (SD) were calculated for continuous variables. Fischer’s exact test was used to compare patients with and without OI.
Results: A total of 219 patients with RP (Penn=117; NIH=102) were included; of which, 185 (84%) were female, 194 (89%) were white, average age was 43 (SD 12.9) and average disease duration was 6.9 (SD 10) years. One hundred five (48%) had an OI during their disease course: episcleritis (n=43, 41%), scleritis (n=37, 35%), and uveitis (n=23, 22%), and recorded only in the Penn cohort were conjunctivitis (n=5, 9%) and eyelid swelling (3, 5%). Some patients had more than one OI (Figure 1). Clinical data at the time of diagnosis of RP was available in 117 patients (Penn cohort); 21 (18%) patients had an OI at the time of diagnosis, and the remaining 35 (30%) patients developed OI later. Among the patients with OI, scleral thinning and blindness were observed in 3 (7%) and 1 (2%) patients, respectively. Compared to patients without OI, those with OI had higher rates of fever (n=24, 27%; vs n=15, 12%; p=0.007), arthritis (n=57, 63%; vs n=61, 47%; p=0.020), rash (n=32, 36%; n=15, 12%, p< 0.001), oral ulcers (n=29, 32%; n=25, 19%; p=0.038), genital ulcers (n=20, 22%; n=10, 8%; p=0.003), cough (n=56, 62%; n=58, 45%, p=0.010), and wheezing (n=31, 34%; n=26, 20%, p=0.020). OI was also associated with increased rates of sensorineural hearing loss (SNHL) (n=30, 33%; n=26, 20%, p=0.040), auricular deformity (n=16, 18%; n=7, 5%; p=0.006), and nasal bridge collapse (n=16, 18%; n=8, 6%; p=0.009). Coexisting autoimmune diseases were reported in 32 (27%) patients in the Penn Cohort, with no significant difference between those with and without OI (n=10, 24%; n=22, 29%; p=0.650).Use of non-biologic IS was significantly higher (n=79, 88%; n=95, 74%; p=0.010) in those with OI compared to those without OI. Patients with OI were more likely to receive infliximab compared to those without OI (n=22, 24%; n=10, 8%; p< 0.001). There was no significant difference in the use of GC in patients with and without OI (n=82, 91%; n=121, 94%, p=0.560). (Table 1).
Conclusion: OI is common in RP and often develops after diagnosis, with many patients experiencing multiple ocular manifestations. OI is associated with a higher burden of systemic disease, greater risk of organ damage, and frequent use of non-biologic IS and select biologic IS. These findings underscore the importance of monitoring for OI in RP, which may indicate severe disease and influence treatment decisions.
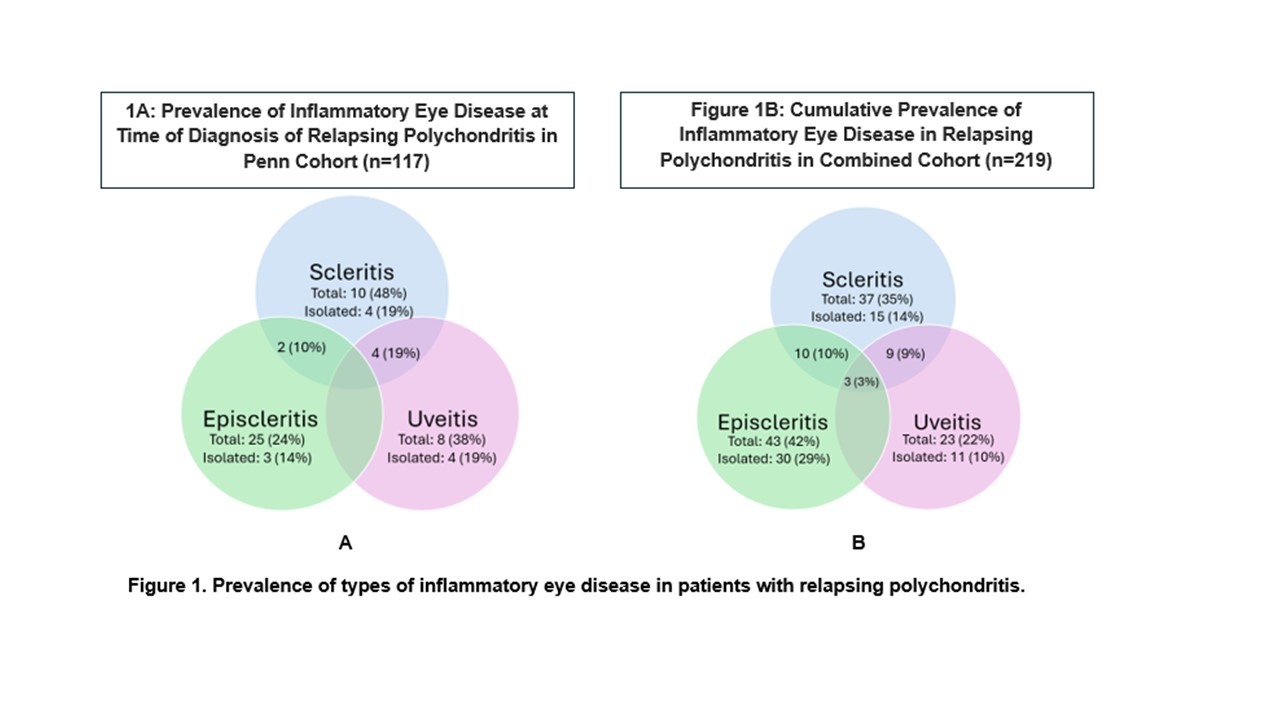 Figure 1. Prevalence of types of inflammatory eye disease in patients with relapsing polychondritis.
Figure 1. Prevalence of types of inflammatory eye disease in patients with relapsing polychondritis.
.jpg) Table 1. Medication use in patients with relapsing polychondritis with and without ocular disease
Table 1. Medication use in patients with relapsing polychondritis with and without ocular disease
To cite this abstract in AMA style:
Gupta A, Rhee R, Quinn K, Amudala N, Bhatt N, McAlear C, ferrada M, Grayson P, Merkel P, Banerjee S. Ophthalmic Manifestations of Relapsing Polychondritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/ophthalmic-manifestations-of-relapsing-polychondritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ophthalmic-manifestations-of-relapsing-polychondritis/
