Session Information
Session Type: Abstract Session
Session Time: 12:45PM-1:00PM
Background/Purpose: RA and PsA follow different pathomechanisms and incur disease-specific erosive and osteoproliferative bone changes. We used data from a large cohort of RA and PsA patients who underwent high-resolution peripheral quantitative computed tomography (HR-pQCT) imaging and analyzed the impact of the primary disease, disease activity and exposure to targeted treatments on bone density, structure and biomechanics over time.
Methods: The study included RA patients fulfilling the 2010 ACR/EULAR criteria and PsA patients fulfilling the CASPAR criteria in University Hospital Erlangen with ethics approval (324_16B) and written informed consent of the participants. HR-pQCT of the distal radius and 2nd and 3rd metacarpal heads (MCP) was performed bi/annually measuring volumetric bone density (vBMD), trabecular and cortical microstructure, bone stiffness and failure load. Cohort follow-up started at the earliest HR-pQCT and ended at the latest. Imaging episodes between consecutive imaging dates were classified based on the type of coinciding targeted treatments and using time-weighted average DAS-28 as the disease activity exposed. HR-pQCT measurements at the beginning and end of an episode were the episode baseline and outcome values. We used mixed-effects/additive regression to model episode outcome as a function of the episode baseline, episode duration, gender, age and weight of the patients and calculated adjusted marginal means at yearly intervals by diagnosis, and at fixed DAS-28 ESR values representing continuous remission (2.0) and continuous high disease activity (6.0). btsDMARD effects were summarized using their regression coefficients comparing to no use.
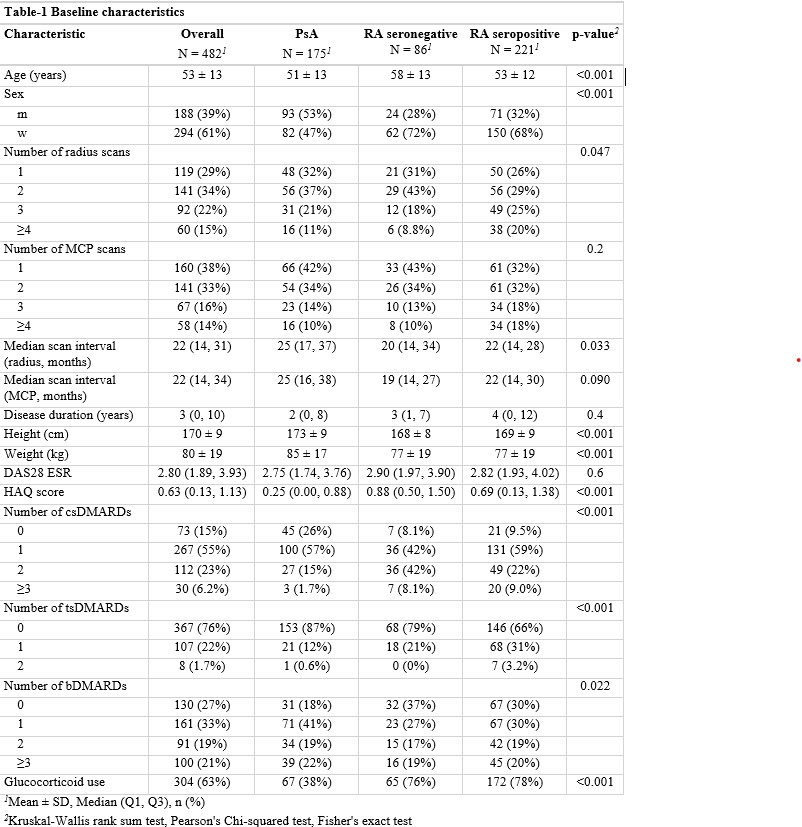
Results: We included 946 radius and 916 MCP scans from 482 patients with PsA (n=175), RA- (n=86) and RA+ (n=221) over a median (IQR) follow-up of 28 months (12 to 50). Glucocorticoid exposure was similar in RA+ and RA- patients (Table-1). Measurements at radius showed a total vBMD deterioration in a similar fashion for both RA and PsA while RA+ patients show lower total vBMD at all timepoints. This separation was prominent in trabecular vBMD (Fig1A) trabecular microstructure (Fig1B) and biomechanics (Fig1C). Patients with PsA showed higher cortical vBMD and a numerically slower rate of cortical bone loss compared to RA (Fig1A) and a stable trabecular count (Fig1B). Patterns at the MCP region were grossly similar. Disease activity comparisons indicate deteriorating radial trabecular vBMD in PsA patients after 1 year under high disease activity and in all vBMDs in RA+ patients after 1 year including stiffness and failure load (Fig2A). TNF blockers, baricitinib and rituximab use improved bone density at the MCP in RA+ patients (Fig2B) , no particular pattern was discernible at the radius and for RA- and PsA.
Conclusion: Seropositive RA patients show worse bone density and microstructure across the board, which is also affected by disease activity, segregating from seronegative RA despite similar glucocorticoid use. Intervention with TNF-blockers, rituximab and baricitinib seem beneficial for bone density at the MCP, possibly indicating interception of local inflammation.
.jpg) Fig1 Marginal mean HR-pQCT measurements over time adjusted for age, gender and weight by diagnosis showing A) Bone density B) Trabecular microstructure, and C) Bone biomechanics.
Fig1 Marginal mean HR-pQCT measurements over time adjusted for age, gender and weight by diagnosis showing A) Bone density B) Trabecular microstructure, and C) Bone biomechanics.
.jpg) Fig2. A) Bone density and biomechanics at the radius in seropositive RA patients assuming constant DAS-28 remission vs. high disease activity over time. B) Regression coefficients indicating the effect of targeted treatments on bone density at the MCP in seropositive RA patients.
Fig2. A) Bone density and biomechanics at the radius in seropositive RA patients assuming constant DAS-28 remission vs. high disease activity over time. B) Regression coefficients indicating the effect of targeted treatments on bone density at the MCP in seropositive RA patients.
To cite this abstract in AMA style:
Tascilar K, Temiz A, Fagni F, Kleyer A, Schuster L, Kemenes S, Bayat S, Simon D, Schett G. Impact of autoimmunity, disease activity and treatment on the time course of bone density, microstructure and biomechanics in inflammatory arthritis. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/impact-of-autoimmunity-disease-activity-and-treatment-on-the-time-course-of-bone-density-microstructure-and-biomechanics-in-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-autoimmunity-disease-activity-and-treatment-on-the-time-course-of-bone-density-microstructure-and-biomechanics-in-inflammatory-arthritis/