Session Information
Date: Wednesday, October 29, 2025
Title: Abstracts: Pediatric Rheumatology – Clinical III (2675–2680)
Session Type: Abstract Session
Session Time: 12:15PM-12:30PM
Background/Purpose: Once clinically inactive, many patients with oligoarticular (oligoJIA) or polyarticular JIA (polyJIA) are interested in de-escalating therapy in a safe and successful manner. Many studies have attempted to answer questions regarding JIA medication withdrawal such as priority of medication to wean on those using combination therapy or recapturing patients who flare. However, no studies to date have attempted to determine if there is an association between duration of medication taper and time to relapse should it occur.
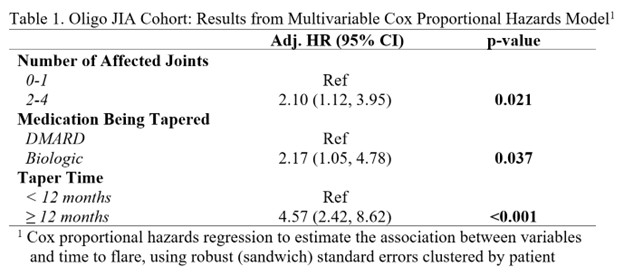
Methods: This is a single site, retrospective cohort study. Eligible subjects included all pediatric patients with oligoJIA or polyJIA seen between January 1, 2015, and August 31, 2023, who tapered off a unique conventional disease-modifying antirheumatic drug (cDMARD), which included methotrexate or leflunomide, and/or biologic disease-modifying antirheumatic drug (bDMARD), which included adalimumab, infliximab or etanercept, as directed by their rheumatology provider or on their own accord. The primary objective was to determine if there was an association between length of medication taper and time to disease relapse should it occur. The secondary objective was to identify risk factors for JIA disease relapse. Kaplan-Meier survival curves were used to illustrate the observed probability of flare-free survival over time. To explore Unadjusted Cox proportional hazards regressions were used to estimate the association between exposures of interest and time to flare, using robust (sandwich) standard errors clustered by participant (due to multiple tapers within certain subjects). Variables that were statistically significant in the unadjusted models were entered into a final multivariable model.
Results: Among oligoJIA subjects (n = 67), there were 60 unique cDMARD tapers, 17 unique bDMARD tapers, and one patient simultaneously tapered cDMARD and bDMARD, who was excluded from the analysis. Risk factors (p< 0.05) for oligoJIA flare included tapering off a bDMARD, having more than 1 joint affected, HLA-B27 and RF positivity. Subjects with longer tapers ( >6 months, > 12 months) of either medication class demonstrated increased risk for disease relapse compared to shorter taper durations (HR of 2.29 (95%CI: 1.23-4.26, p=0.009) for >6 months, HR of 6.41 (95% CI: 3.47-11.76, p< 0.001) for > 12 months). Among polyJIA subjects (n = 41), there were 41 unique cDMARD tapers and 10 unique bDMARD tapers. Risk factors for polyJIA flare included tapering off a bDMARD and abruptly stopping either JIA medication (versus tapering over time). Subjects with longer taper durations (≥1 day) demonstrated a protective effect against disease relapse compared to subjects who immediately stopped (aHR: 0.41; 95% CI: 0.016-1.07, p=0.035).
Conclusion: For oligoJIA patients, there was an inverse association between duration of medication taper and time to relapse. This suggests that children with clinically inactive oligoJIA and particularly those with favorable factors (negative RF or HLA-B27 status, cDMARD monotherapy, only one joint affected) could undergo faster tapers. However, in those with polyJIA, children may benefit from a taper over time versus abruptly stopping their medication.
To cite this abstract in AMA style:
Oliveros C, Rouster-Stevens K, Johnson L, Prahalad S. The Association Between Medication Taper Duration and Time to JIA Disease Flare: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-association-between-medication-taper-duration-and-time-to-jia-disease-flare-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-medication-taper-duration-and-time-to-jia-disease-flare-a-retrospective-cohort-study/

.jpg)
.jpg)