Session Information
Session Type: Abstract Session
Session Time: 3:30PM-3:45PM
Background/Purpose: The role of lung ultrasound (LUS) in assessing disease severity of interstitial lung disease (ILD) remains unclear. We employed a semiquantitative scoring system to evaluate the ability of a LUS score to assess disease severity in patients with connective tissue disease (CTD) related ILD.
Methods: This study involved individuals from a prospective cohort of patients with CTD exhibiting respiratory symptoms or clinical suspicion of ILD who attended our hospital from December 2023 to December 2024. All patients underwent LUS, high-resolution CT (HRCT), and pulmonary function test (PFT) within one week. LUS was performed using a 14 intercostal scanning protocol, and the total LUS score was calculated using a semiquantitative scoring system (Figure 1). HRCT results were evaluated by two experienced radiologists and analyzed a commercial quantitative computed tomography (QCT) software. According to the Goh staging system, ILD was categorized as limited or extensive if < 20% or >20%, respectively, of the total lung area was affected. Differences in LUS scores across ILD severity groups were compared, and correlations between LUS scores and QCT and PFT results were analyzed. The stratification efficacy of the LUS score was evaluated using the area under of the receiver operating characteristic curve (AUC) with 95% confidence intervals (CI).
Results: A total of 146 patients with CTD-ILD were enrolled (mean age 56.1 ± 11.7 years; 108 [74.0%] female). Among these patients, 50 (34.2%) were diagnosed with idiopathic inflammatory myopathy; 35 with rheumatoid arthritis; 27 with Sjögren’s disease; 20 with systemic sclerosis; 11 with systemic lupus erythematosus; and 3 with mixed connective tissue disease. The cohort comprised 30 individuals classified with preclinical ILD, 76 with limited ILD, and 40 with extensive ILD. Patients with extensive ILD exhibited higher QCT parameters but lower PFT results than those with limited ILD or preclinical ILD. The median LUS scores in patients with extensive ILD were significantly higher (72, IQR 62‒77) compared with those in the limited ILD (43, IQR 24.5‒58.5) and preclinical ILD groups (8.5, IQR 3.0‒18.75) (P < 0.001). Furthermore, LUS scores exhibited a positive correlation with fibrosis extent assessed by QCT (r = 0.776, P < 0.001) and negative correlations with diffusion capacity for carbon monoxide (DLCO) (r= -0.533, P < 0.001) and forced vital capacity (FVC) (r = -0.524, P < 0.001) (Figure 2). At cutoffs of 19.5 and 55.5, LUS distinguished preclinical ILD from limited ILD and extensive ILD, with sensitivities of 95.7% and 89.7% and specificities of 83.3% and 73.8%, respectively (AUC 0.963 and 0.877) (Figure 3). The agreement between LUS and HRCT severity stratification was good (quadratic weighted kappa = 0.736; 95% CI: 0.621‒0.850), and interoperator consistency was excellent (intra-class correlation coefficient: 0.971, 95% CI: 0.965‒0.980, P < 0.001).
Conclusion: LUS exhibited favorable sensitivity and specificity for distinguishing between CTD-ILD patients of varying severity grades. Moreover, LUS presents a promising imaging modality for disease severity stratification and longitudinal monitoring of disease progression.
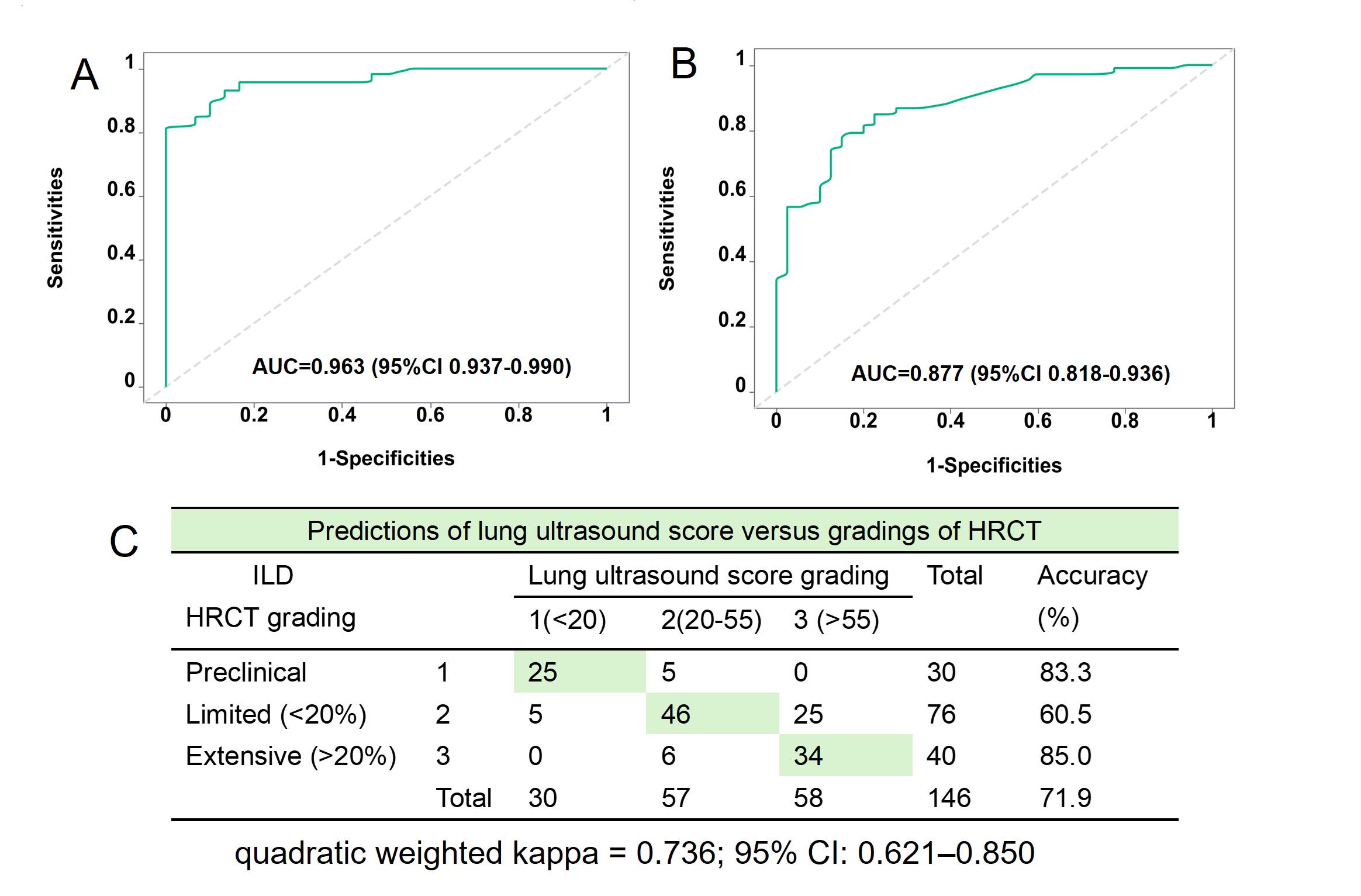 Figure 1.The bilateral anterolateral posterior chest wall 14 intercostal lung ultrasound scanning method (A) and a lung ultrasound scoring system (B) for connective tissue disease related interstitial lung disease.
Figure 1.The bilateral anterolateral posterior chest wall 14 intercostal lung ultrasound scanning method (A) and a lung ultrasound scoring system (B) for connective tissue disease related interstitial lung disease.
.jpg) Figure 2. Differences in lung ultrasound scores among patients with connective tissue diseases related interstitial lung diseases of varying HRCT severity grading (A), as well as correlation between lung ultrasound scores and fibrosis extent on quantitative HRCT (B), predicted percentage of forced vital capacity (C), and predicted percentage of diffusing capacity of the lungs for carbon monoxide (D) in patients.
Figure 2. Differences in lung ultrasound scores among patients with connective tissue diseases related interstitial lung diseases of varying HRCT severity grading (A), as well as correlation between lung ultrasound scores and fibrosis extent on quantitative HRCT (B), predicted percentage of forced vital capacity (C), and predicted percentage of diffusing capacity of the lungs for carbon monoxide (D) in patients.
.jpg) Figure3. Receiver operating characteristic curves of lung ultrasound scores for distinguishing between preclinical ILD and ILD (A), as well as between limited and extensive ILD (B); and the predictions of lung ultrasound score versus HRCT gradings (C). AUC: area under the receiver operating characteristic curve.
Figure3. Receiver operating characteristic curves of lung ultrasound scores for distinguishing between preclinical ILD and ILD (A), as well as between limited and extensive ILD (B); and the predictions of lung ultrasound score versus HRCT gradings (C). AUC: area under the receiver operating characteristic curve.
To cite this abstract in AMA style:
ding j, zhang y, Pang L, guo n, zheng z. Exploring the Role of a Lung Ultrasound Score in the Assessment of Severity of Connective Tissue Disease-Related Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/exploring-the-role-of-a-lung-ultrasound-score-in-the-assessment-of-severity-of-connective-tissue-disease-related-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/exploring-the-role-of-a-lung-ultrasound-score-in-the-assessment-of-severity-of-connective-tissue-disease-related-interstitial-lung-disease/
