Session Information
Date: Tuesday, October 28, 2025
Title: Abstracts: Systemic Lupus Erythematosus – Etiology and Pathogenesis (2597–2602)
Session Type: Abstract Session
Session Time: 1:15PM-1:30PM
Background/Purpose: Current therapies for cutaneous lupus erythematosus (CLE) are limited, highlighting the need for novel approaches. CLE lesions commonly exhibit photosensitivity and heightened type I interferon (IFN) activity. Persistent type I IFN exposure amplifies the inflammatory response of keratinocytes (KCs) to ultraviolet (UV) radiation, triggering further IFN production and worsening skin lesions. Interactions between KCs and other skin cells, such as melanocytes, are key to modulating inflammation and providing protection against environmental stressors. In this study, we investigated novel regulatory pathways between KCs and melanocytes.
Methods: We performed single-cell RNA sequencing (scRNA-seq) to characterize gene expression in melanocyte populations derived from skin biopsies of systemic lupus erythematosus (SLE) patients and healthy individuals, both with and without UV exposure. To investigate keratinocyte–melanocyte interactions, primary keratinocytes were treated with UV radiation, IFN-α, or a combination of both. The resulting conditioned media were applied to primary melanocytes along with specific inhibitors targeting JAK1 (Baricitinib), STING (H151), or cGAS (G140). MHC class II and pro-inflammatory cytokine expression in melanocytes were assessed via RT-qPCR. In parallel, cytokine profiles of the keratinocyte supernatants were analyzed using the Luminex Human Discovery Assay to identify soluble factors that may contribute to melanocyte activation.
Results: Analysis of single-cell RNA sequencing data identified leukemia inhibitory factor (LIF) as a key upstream regulator in SLE keratinocytes, with elevated LIF expression observed in primary keratinocytes. Supernatants from UV-treated keratinocytes induced upregulation of antigen-presenting markers in melanocytes in a JAK1-dependent manner. Given that LIF signals through the LIF receptor to activate the JAK-STAT pathway, we hypothesized that LIF would promote inflammatory responses in melanocytes. Unexpectedly, however, the addition of LIF to keratinocyte supernatants significantly reduced MHC-II expression in primary melanocytes.
Conclusion: Melanocytes isolated from SLE lesions exhibit abnormal features, including heightened type I interferon exposure and upregulation of MHC class II molecules. Our data suggest that type I IFNs drive this upregulation and may shift melanocyte function away from pigmentation and keratinocyte support toward immune activation. Importantly, we show that the addition of LIF or JAK1 inhibitor significantly suppresses MHC-II expression in melanocytes, revealing potential regulatory pathways that may limit aberrant immune activation in CLE. Cytokine profiling confirmed that LIF is actively secreted by keratinocytes and modulated in inflammatory conditions. These findings support a model in which LIF acts as a brake on IFN-driven immune activation, a function that may be compromised in lupus skin, contributing to aberrant immune activation. Ongoing studies aim to further define the role of LIF in CLE.
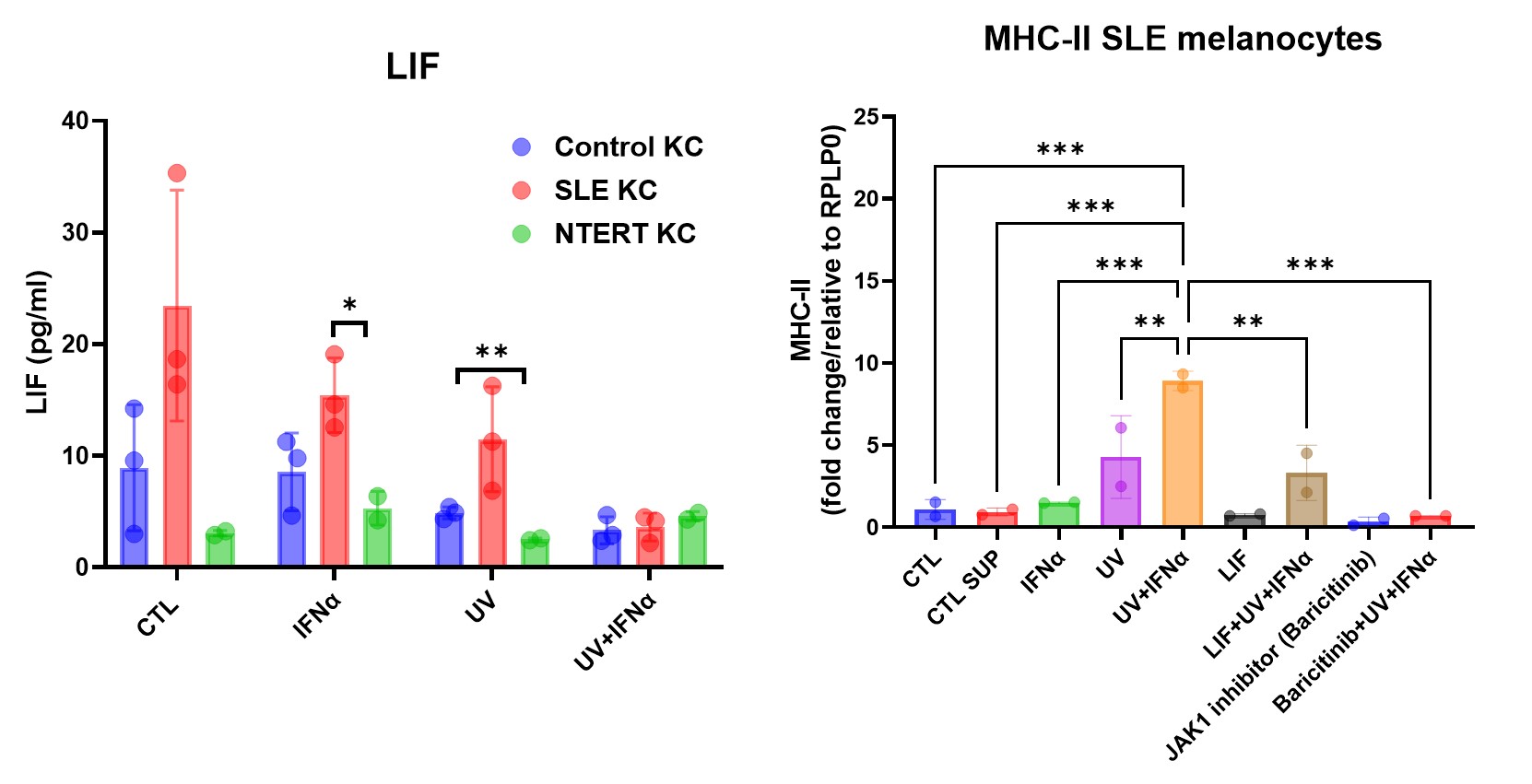 Figure 1. LIF attenuates MHC-II expression in melanocytes stimulated with UV/IFN-α–treated keratinocyte supernatants. (a) Primary keratinocytes from healthy controls (HC), SLE patients, and NTERT KC cells were exposed to IFN-α, UV, or UV+IFN-α. LIF levels in the supernatants were quantified using the Luminex Human Discovery Assay. SLE keratinocytes showed a significant reduction in LIF secretion following UV+IFN-α treatment. (b) Primary melanocytes were stimulated with keratinocyte-conditioned media from the indicated treatments. Supernatants from UV+IFN-α–treated KCs strongly induced MHC-II expression in melanocytes, which was significantly reduced by the addition of LIF (250ng/ml) or JAK1 inhibitor (5uM). MHC-II levels were measured by RT-qPCR. *P ≤ 0.05, **P ≤ 0.01, **P ≤ 0.001.
Figure 1. LIF attenuates MHC-II expression in melanocytes stimulated with UV/IFN-α–treated keratinocyte supernatants. (a) Primary keratinocytes from healthy controls (HC), SLE patients, and NTERT KC cells were exposed to IFN-α, UV, or UV+IFN-α. LIF levels in the supernatants were quantified using the Luminex Human Discovery Assay. SLE keratinocytes showed a significant reduction in LIF secretion following UV+IFN-α treatment. (b) Primary melanocytes were stimulated with keratinocyte-conditioned media from the indicated treatments. Supernatants from UV+IFN-α–treated KCs strongly induced MHC-II expression in melanocytes, which was significantly reduced by the addition of LIF (250ng/ml) or JAK1 inhibitor (5uM). MHC-II levels were measured by RT-qPCR. *P ≤ 0.05, **P ≤ 0.01, **P ≤ 0.001.
To cite this abstract in AMA style:
Moallemian R, Zhang L, Gharaee-Kermani M, Holle R, Kahlenberg J. Keratinocyte-Secreted Leukemia Inhibitory Factor Counteracts Type I IFN-Induced Antigen-Presenting Phenotype in Melanocytes: Utility in Cutaneous Lupus Skin [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/keratinocyte-secreted-leukemia-inhibitory-factor-counteracts-type-i-ifn-induced-antigen-presenting-phenotype-in-melanocytes-utility-in-cutaneous-lupus-skin/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/keratinocyte-secreted-leukemia-inhibitory-factor-counteracts-type-i-ifn-induced-antigen-presenting-phenotype-in-melanocytes-utility-in-cutaneous-lupus-skin/
