Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Outcomes for ANCA associated vasculitis (AAV) have been transformed in recent years with many patients achieving prolonged periods of remission. Guidelines advise continuing maintenance therapy following initial treatment for at least 24-48 months but beyond this there is debate in balancing the risks of disease relapse against those of prolonged immunosuppression. These decisions could be guided by biomarkers to identify patients who are likely to remain in remission or could predict incipient flare at an early stage. In this study we explored the utility of serum proteomics measured from patients in clinical remission to predict their risk of future relapse.
Methods: Serum samples and matched clinical data from participants with MPO- or PR3-ANCA+ AAV were retrieved from an ongoing prospective cohort study at Mass General Brigham. The levels of 92 circulating proteins were measured using the Olink inflammation proteomic assay. Relapse was defined as a change in clinical symptoms prompting new or modified treatment after achieving initial remission, and for those patients, additional information was collected including creatinine, presence of sinopulmonary symptoms, and treatment provided during relapse. Proteomic data from the population who experienced relapse was compared to control populations those who did not experience relapse to identify significant changes in protein expression as compared via unpaired t-tests. Adjustment for multiple comparisons was based on the 10% false discovery rate (FDR) procedure.
Results: We identified 44 patients who were in remission when serum was sampled for proteomic analysis. This cohort was balanced for sex (55% female) and ANCA specificity (50% MPO-ANCA) (Table 1). Over the follow-up period 29.5% of patients (n=13) experienced at least one flare. The commonest manifestation of flare was sinopulmonary involvement (77%) (Table 2). The only baseline clinical predictor of future flare was male sex (p=0.04), whereas neither age (p=0.12) nor ANCA subtype (p=0.90) was predictive. There were higher rates of relapse in those who received cyclophosphamide (46% vs 29%) and lower levels in those who received Rituximab (55% vs 15%), but neither was statistically significant (Table 2). Proteomic analysis revealed that elevated levels of the IL6-family cytokine Oncostatin M (OSM) during remission was significantly associated with future risk of flare (adjusted p value < 0.001) (Figure 1).
Conclusion: For many patients with AAV the most pressing clinical dilemma is identifying when treatment can safely be withdrawn. In deriving a biomarker serum proteomics are an attractive modality because sampling is minimally invasive, assays are robust and can be captured longitudinally. In this preliminary study we identify the IL-6 family cytokine OSM as being predictive of future flare. This is consistent with our previous analysis that has found that OSM is significantly raised in active AAV. While the number of patients in our cohort who flared was low, this study supports the potential of this approach. Our future work will expand this cohort and explore the effect of treatment and whether longitudinal changes can enhance its predictive power.
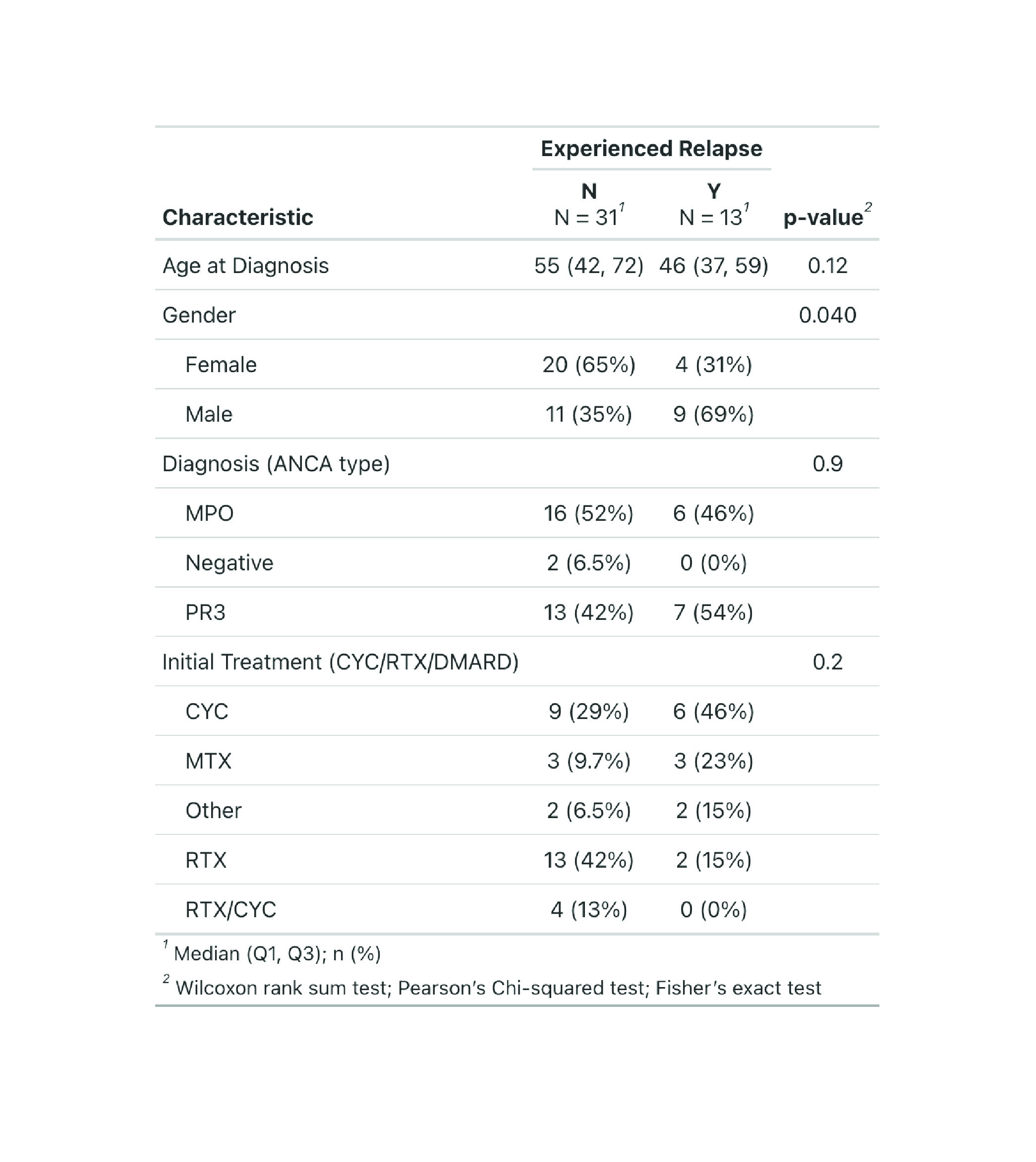 Table 1: Characteristics of total sample population
Table 1: Characteristics of total sample population
.jpg) Table 2: Comparison of patients who experienced relapse versus those with sustained remission
Table 2: Comparison of patients who experienced relapse versus those with sustained remission
.jpg) Figure 1: (A) Volcano plot of proteomic expression data of Olink inflammatory panel proteins. (B) Table summarizing the top 5 differentially expressed proteins between the population experiencing relapse versus the population maintaining prolonged remissions with uncorrected p values and FDR adjusted p-values
Figure 1: (A) Volcano plot of proteomic expression data of Olink inflammatory panel proteins. (B) Table summarizing the top 5 differentially expressed proteins between the population experiencing relapse versus the population maintaining prolonged remissions with uncorrected p values and FDR adjusted p-values
To cite this abstract in AMA style:
Barnes E, Shepherd N, Johnson C, O'Dea D, Jiang B, Hyle E, Williams Z, Wallace Z, Reynolds G. Predicting future relapse with proteomics in ANCA-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/predicting-future-relapse-with-proteomics-in-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predicting-future-relapse-with-proteomics-in-anca-associated-vasculitis/
